Page 1 (0s)
CHILDHOOD IMMUNIZATION AND ETHICAL ISSUES. BY SHEHAN MALONEY.
Page 2 (9s)
Immunization is a process by which a person becomes protected against through vaccination. As a result, immunization have been major force reducing the occurrence of disease globally. The global immunization program has controlled and eliminated following diseases from the world such as polio, tetanus, malaria, etc. However, despite these benefits a lot of ethical issues surround immunizations. The Immunisation Australia was implemented in 1997, with the aim of increasing uptake of childhood immunisations. The Strategies introduced included school entry immunisation requirements and a series of financial incentives for parents and general practitioners..
Page 3 (11s)
The coverage increased rapidly, from an estimated 53% in the 1980s to over 90%. In presently, the childhood vaccination coverage is almost 95%. This figure reflects the nation’s commitment to an accountability in disease prevention, not only within the country but also throughout the Western Pacific Region, where certain VPDs (for example, the rubeola virus) remain prevalent in some locations. When viewed collectively, the current Australian childhood coverage rates are reported to be 95% or above. However, these figures can mask coverage deficits seen in specific sub-populations and in certain geographical locations..
Page 4 (12s)
In Australia, childhood vaccination levels have increased substantially in the past few decades. Despite high overall vaccination coverage, pockets of under immunisation exist; with an increase in measles cases over the last 5 years. In both the media and the scientific literature, vaccine hesitancy has been the main focus when tackling these issues. However, vaccine hesitancy is only part of the explanation. Recent studies from Australia and Europe have shown social inequities to be more important predictors of vaccination coverage levels. The Australian study showed that the majority of incompletely vaccinated infants did not belong to a family rejecting vaccines, but to parents who were experiencing socioeconomic barriers to immunisation..
Page 5 (14s)
Pockets of under-immunised groups are a serious threat to controlling the spread of vaccine preventable diseases such as measles. Outbreaks of measles have been reported in the past decade in many countries among groups of non-immunised individuals from certain ethnic groups and children of parents with certain religious beliefs Measles among the under-immunised groups can put vulnerable children, such as infants that are too young for measles vaccination and individuals with immune deficiencies, at risk. Studying the social distribution of vaccination coverage is therefore crucial in identifying these pockets of under immunised groups and preventing future outbreaks..
Page 6 (15s)
According to the UN’s Sustainable development goals, the issue of under immunisation is not only about differential impact of disease on vulnerable children, but also about the crucial goal of no child being left behind. This requires identifying current social inequalities in vaccination coverage and assessing possible macro-level factors that could be playing a role in the observed patterns, such as the structure and organisation of healthcare services, vaccination policies, strategic immunisation plans, and the funding of vaccination programmes. Even in countries with universal free vaccination programs, there is inequitable vaccination coverage. In Australia, all childhood vaccinations that are part of the National Immunisation Program (NIP) are free-of-charge..
Page 7 (17s)
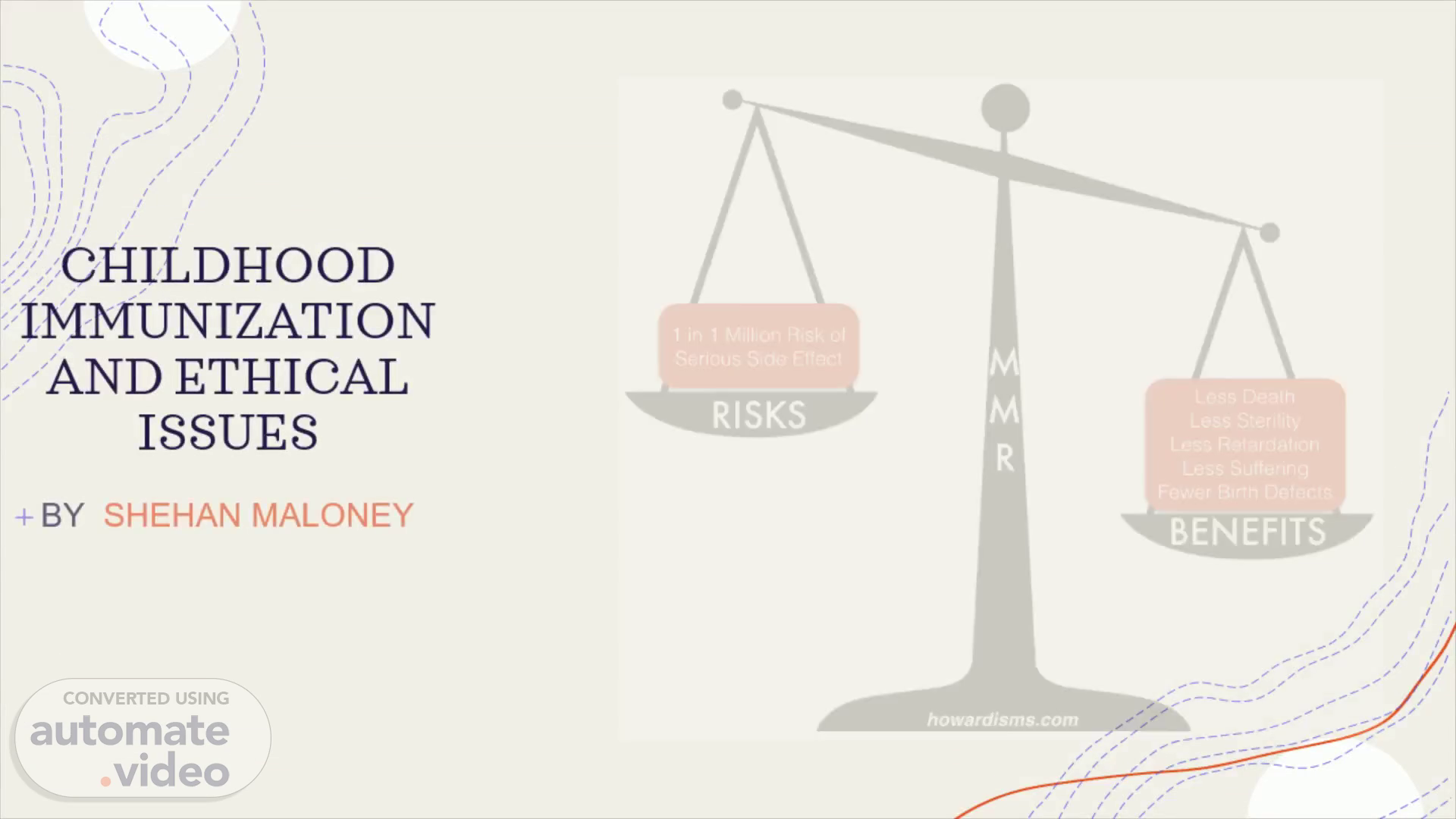
See the source image.
Page 8 (18s)
The several national reports have shown the Aboriginal population to have lower levels of measles-mumps-rubella (MMR) vaccination coverage when compared to the national average. Furthermore, several studies have analysed other socio-economic factors and found them to be of importance for vaccination coverage. However, there is still a gap in knowledge regarding the size and trends in social differences for MMR vaccination coverage with respect to other factors and whether there are regional differences..
Page 9 (19s)
In wealthier countries, the ethical issues that surround vaccination tend to focus on the rights of individuals versus government or society. In poorer countries, the fundamental issue is the lack of access to basic necessities for health, such as adequate nutrition, clean water, medicines or vaccines. Although poverty is clearly the main cause of these deficiencies, other factors contribute, such as the low priority given to health and preventive measures, lack of political and economic power of the people most affected (children and women), corruption and regional warfare..
Page 10 (21s)
From my perspective I strongly believe that vaccinations not only protect your child from deadly diseases, such as polio, tetanus, and diphtheria, but they also keep other children safe by eliminating or greatly decreasing dangerous diseases that used to spread from child to child. A vaccine is a dead, or weakened version, or part of the germ that causes the disease in question. When children are exposed to a disease in vaccine form, their immune system, which is the body's germ-fighting machine, is able to build up antibodies that protect them from contracting the disease if and when they are exposed to the actual disease..
Page 11 (22s)
Over the years, vaccines have generated some controversy over safety, but no convincing evidence of harm has been found. And although children can have a reaction to any vaccine, the important thing to know is that the benefits of vaccinations far outweigh the possible side effects..