Page 1 (0s)
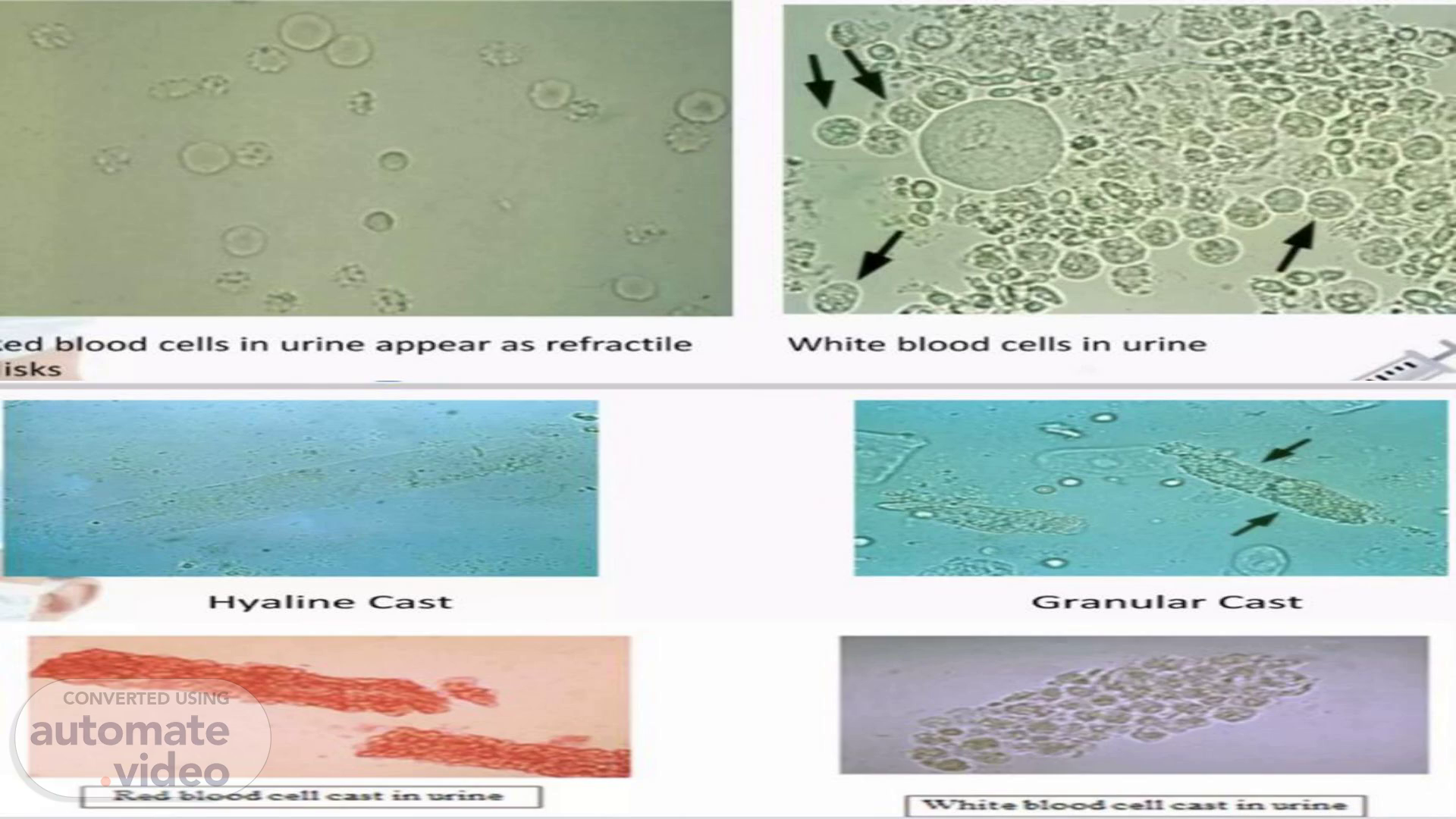
ed blood cells in urine appear as refractile isks Hya I i Cast White blood cells in urine G ra u r Cast c.a.•e.
Page 2 (9s)
NORMAL CRYSTALS Ca Phosphate Leucine.
Page 3 (15s)
Abnormal Per High Power Field (HPF) (400x) ⁃ > 3 erythrocytes ⁃ > 5 leukocytes ⁃ > 2 renal tubular cells ⁃ > 10 bacteria The chemical analysis of urine us undertaken to evaluate the levels of the following components: ⁃ Protein ⁃ Glucose ⁃ Ketones ⁃ Occult blood ⁃ Bilirubin ⁃ Urobilinogen ⁃ Bile salts.
Page 4 (27s)
Collection: • Universal Precautions • Stool should be collected in a dry, sterilized, wide mouthed container. • It should be uncontaminated with Urine or any other body secretions. • Properly named and always a fresh sample should be tested. PARASITE: • Round worm • Hook worm • lape worm • Pin worm • Whipworm Microscopic examination A. MATERIALS • Microscope slides • Cover slips • Sodium chloride solution • Lugol's lodine Solution • Wooden applicator • Fresh stool • Gloves B. SLIDE PREPARATION • 1 drop of NACL on slide • Specimen.
Page 5 (47s)
Table 2. Common parasites detected on stool examination haematobium, Hymenolepis Pathogenic Nematodes scaris lumbricoides Hookworm (Necator americanus & Ancylostoma duodenale) Trichuris trichiura Strongyloides stercoralis Controversial Protozoa Dientamoeba fragilis (diarrhea) Entamoeba olecki (diarrhea) Other Nonpathogenic Protozoa rematodes Schistosoma (S. mansoni, S. japonicum) Other flukes (Ophisthorchis spp.) Fasciola, Paragonimus westermani) estodes Taenia solium Taenia. saginatum nana Protozoa Entamoeba histolytica* Giardia intestinalis (also known s G. lamblia duodenalis) Blastocystis Entamoeba hominis dispar* (diarrhea) Entamoeba moshkowskii* Entamoeba coli Entamoeba hartmanii Endolimax nana Iodamoeba utschlii Chilomastix mesnili *The cyst of E. histolytica E. dispar and E. moshkowskii are morphologically identical by stool microscopy.
Page 6 (1m 3s)
Parasites found in urine • Trichomonas vaginaljs— Protozoa • Sc ist som Causes Sqhistq-so-miasis Wuchereriabancrofti— nematode caus —zip o.
Page 7 (1m 12s)
Occult blood in the stool may indicate colon cancer or polyps in the colon or rectum..
Page 8 (1m 21s)
The fecal immunochemical test (FIT) is used as a screening test for colon cancer. It tests for hidden blood in the stool, which can be an early sign of cancer. FIT only detects human blood from the lower intestines. There are three methods used for the concentration of stool (seen in Hammod hospital) •Formalin-ethyl-acetate concentration method. • Zinc-floatation method. • Sheather sugar floatation method. Stool concentration:.
Page 9 (1m 39s)
Histology and pathology…...
Page 10 (1m 45s)
Medical Histology is the microscopic study of tissues and organs through sectioning, staining, and examining those sections under a microscope. Often called microscopic anatomy and histo-chemistry, histology allows for the visualization of tissue structure and characteristic changes the tissue may have undergone. 1-)Grossing when the histology lab receives tissue specimens we make a macroscopic examination ( description like weight) and we take a small sample . 2- )fixation this small sample we put it in a Cast full with fixative reagent( formalin- formaldehyde) This fixative reagent prevents the sample from making autolysis. Procedure:.
Page 11 (2m 5s)
3- processing ( overnight in machine) this machine contains 12 jars and each jar contains something different from another jar. 1-2 jar contain formaldehyde for fixation 3-4-5 contain increased concentration of alcohol 70%-80%-90% and this for dehydration. 6-7-8 (100%ethanol for pure dehydration) 9-10 contains xylole for clearing 11-12 liquid paraffin. 4-) embedding ( preparation of paraffin block) Contain two plate: 1) hot plate 65•C ( melting of paraffin 56•C) 2) Freeze plate ( to make the paraffin's cold and make a block ) First we put the sample in a cassette and put a hot paraffin inside the cassette. Then we put this cassette on the cold plate to make a block. 4-)Microtome ( preparation of slide) We cut a thin layer by using the microtome Then we put this thin layer in the water bath(40•c) then put the thin layer in the slide..
Page 12 (2m 39s)
5-) staining Steps : 1-xylole 1 ( for clearing for 10min ) 2-Alcohol 2 concentration ( for washing) for 1-2min 3-wash using water for 1-2min 4- hematoxylin ( alkaline stain that stain the nucleus since the dna is acid ) for 12 min 5-wash with water tell the water become clear 6-Acid alcohol ( to remove excess of hematoxylin for a few min) 7- wash with water 8- Ammonia water 9- Eosine ( that stain the cytoplasm) for 2 min 10-3 concentration of ethanol for each jar 1 min ( for dehydration) 11- xylole 2 jar for clearing Xylole 3 jar for clearing 12- we fix a cover slide on the slide 6-) observation under microscopes.
Page 13 (3m 3s)
TP1020 Automabc Tissue Processor Processing EGI 160 Paraffin Embeddi Center Embedding RM223S R VTIOOOS V Cutting Microtorne -blade WORKFLOW PSR Rat heart - bme • Leica CM 1900 Otyrnpt.ß IMT-2 Wcroscope Leca AutoStao« XL.
Page 14 (3m 13s)
Cytology ……...
Page 15 (3m 19s)
Cytology: is the study of the cells. It's mainly used to diagnose or screen for cancer. It's also used to screen for fetal abnormalities, for pap smears, to diagnose infectious organisms, and in other screening and diagnostic areas. Specimen: ● Urine ● CSF ● Pleural fluid ● Bronchial aspirate ● Sputum ● Pap smear ● Vaginal fluid Note: Cytospine is the machine that make centrifuge for the urine and CSF specimens that have a low concentration of cell and this cell are sedmented directly on the slide..
Page 16 (3m 42s)
we make a Pap smear to detect cervical cancer ( HPV) . And other things like inflammation and abnormalities in the reproductive system were also detected Specimen obtained by using vaginal swab The materials are directly fixed in the glass slide and fixed with alcohol 95% for 15-30 min ..
Page 17 (3m 55s)
A new method of preparing cervical samples for cytological examination. Unlike the conventional 'smear' preparation, it involves making a suspension of cells from the sample and this is used to produce a thin layer of cells on a slide. We take a sample of cells from the cervix and place them into a liquid solution that preserves the cell . The machine removes the excess blood, mucous and inflammatory cells and we get a thin layer of cells in the glass slide. The cell is stained and examined under a microscope..
Page 18 (4m 16s)
Fine-needle aspiration (FNA) uses a needle and syringe to get a tissue or fluid sample from a suspicious mass in your body. Healthcare providers use it to help diagnose abnormal tissue in several areas of your body, such as your breasts, thyroid and lymph nodes. Staining use in cytology: 1. fixation and rehydration with alcohol (95%, 70%) for 5 min 2. Wash with water 3. Hematoxylin for 5 min that stain the nucleus 4. Wash with water 5. Acid alcohol for 5 min to remove the excess of hematoxylin stain 6. Wash with water for 2 min 7. Alcohol for 1 min 8. Orang G for 5 min ( that stain the cytoplasm) 9. 2 jar that contains different concentrations of alcohol 1 min for each jar 10. Polychrome for 2 min.
Page 19 (4m 47s)
Blood bank…….
Page 20 (4m 53s)
A blood bank is a center where blood gathered as a result of blood donation is stored and preserved for later use in blood transfusion..
Page 21 (5m 3s)
● Whole blood, which is blood transfused without separation. Red blood cells or packed cells are transfused to patients with anemia/iron deficiency. It also helps to improve the oxygen saturation in blood. It can be stored at 2°C-6°C or 4°C for 35–45 days with mannitol without mannitol 24 days. ● Platelet transfusion is transfused to those with low platelet count. Platelets can be stored at 22°C for 4 days. ● Plasma transfusion is indicated to patients with liver failure, severe infections or serious burns. Fresh frozen plasma can be stored at a very low temperature of -20 °C for up to 12 months. The separation of plasma from a donor's blood is called plasma-pheresis. ● Cryoprecipitate: we can obtain this from the FFP. Take the FFP and put it in the refrigerator at 0°C since the plasma becomes liquid at a zero degree but the cryoprecipitate at 4 degree. And then we obtain the cryoprecipitate by this way we can store the cryoprecipitate for 1year (cryoprecipitate contains the clotting factor)..
Page 22 (5m 43s)
In hamood hospital we have a 4 section for the blood bank department: 1. Donation area: the area where the people come to donate. 2. Preparation area: the area where the employees prepare the blood example ( separate of whole blood to packet cell- separate the plasma from the blood) 3. Distribution area: this area where the components store like FFP/ packet cell- platelets…) and in this area the people who need blood or anything from this component come to this area and tell the employee and the employee will give them what they need. 4. Testing area: is this area where the employee makes some test for the blood that recessive from the people . What test is made when we recessive the blood unit ? ● Blood group ● Cross match ● Coombs- direct / indirect.
Page 23 (6m 11s)
In hamood hospital we make the blood group in a card and in this card we have a forward test and reverse test . ● Forward blood test: we have an known antibody and unknown antigen. We put suspension ( blood + diluent ) and the card contains the known antibody. ● Reverse test: unknown antibody and known cell (A cell and B cell) we put cell A and cell B and plasma. But to know if the card is good or not the control must be negative. Results: ●Positive test (agglutination presence at the top of the card) ●Negative (agglutination presence at the bottom of the card) ..
Page 24 (6m 34s)
0/0910 0/0911 YOL 0/091 ezoc 'sssn 0/09'e 0/0178 +11 H 0/011 0 O/ozv O/oev @ SAdÅ1 Noun81us10.
Page 25 (6m 43s)
Cross-matching is a simple and commonly practiced laboratory test that verifies blood compatibility. For example, if an AB positive recipient needs blood and there are no AB positive donors, they could receive blood from a Type B positive donor after a proper cross match. How can I make it ? Add to the tube 1000ul of diluents +10ul of blood from donor, take from it 50ul and put in gel card and mix them with 25ul of plasma from patient Incubate for 15 min and centrifuge for 15 min. a negative result(compatible blood) should be obtained in order to provide the blood unit to the patient..
Page 26 (7m 8s)
The direct Coombs test is used to detect antibodies that are stuck to the surface of red blood cells. An (positive) direct Coombs test means you have antibodies that act against your red blood cells. This may be due to: 1-Autoimmune hemolytic anemia. 2-Chronic lymphocytic leukemia or similar disorder. How can I make it ? We make a blood suspension by mixing 10ul of patient blood with 1000ul of diluents. Take 50ul from them into a gel card. Result: ●Positive result: agglutination presence at the top ( there is an IgG antibody in the surface of RBCs). ●Negative result: agglutination in the bottom of the card. No antibody against the RBCs. Note that the gel cad contains anti- IgG..
Page 27 (7m 35s)
To determine unexpected (irregular) IgG antibodies in patients serum or in the donor serum. How can I make it ? 1-Add 50ul from the Coombs cell (C1,C2,C3) that contain all types of the antigen except ABO system antigen of indirect coombs. 2- Add 50ul of patient plasma into them, then incubate for 15 min and centrifuge for 15 min Agglutination test means presence of irregular antibodies. Used as a screening process to see how you'll react to a blood transfusion. An indirect Coombs test is also routinely given as part of prenatal testing..
Page 28 (7m 56s)
1- The person comes to the donation area and in this area we have a room where the person sits in with the employee and the employee asks the person some questions. ● age 15-60 ● ID: if we don’t have if we don’t take blood ● weight more than 60kg ● tattoo we don’t take blood ● blood pressure normal 120/80 ● If the donor go to dentist ● If the donor travels to a country that has a risk of malaria disease…….
Page 29 (8m 17s)
Questions Are ou feelin health and well toda ? Are you currently taking antibiotic or any other edication for an infection? Are you currently taking or have you ever taken any 2dication for an reason? If es list: In the past 4 hours, have you eaten? In the past 48 hours, have you donated platelets. sma or leukocytes? n the past 7 days, have you had any tooth extraction? n the past 28 days, have you had any fever, infection ludin diarrhea, urina or respirato tract? the past 8 weeks: Have you had any vaccinations or er shots? ave ou donated whole blood? le past 12 months have you: )een pregnant or are you pregnant now? (Female r onl ; males check: I am male a) a surgery, endoscopy or other invasive procedure? lad a blood/blood component transfusion? Yes No.
Page 31 (8m 53s)
After the donation the blood is collected as a whole blood(RBC-WBC-Platelets). We take this for 30 to 60 min to let the defense process take place between the WBC and the bacteria . After one hour we filter the blood then we make centrifuge for 15 min and we obtain the plasma and a packet cell Then we separate the plasma from the packet cell by a machine and after allow the mannitol to go to the bag that contain the packet cell to give it more life. And we make a different test : ● HBV ● HCV ● Anti-HBs ● HBs-Ag ● Syphilis.
Page 32 (9m 18s)
VVhat Happens to Donated Blood? A pint is is at-vd labeled in a is a lab into d i fferent is trans— ferred to has the to 3 stc»red a rmd ready Plate-lets expire in 5 days. cells in 42 days. in 2 years- place orders based is tested to red it is platelets - for trans.
Page 33 (9m 30s)
1. Syncope (fainting): we stop the transfusion process. 2. Seizure: (stop the transfusion-called emergency department-protect donor for hazard- put donor on floor- see the pulse) 3. Hematoma: bleeding in the large vessels we stop the blood transfusion 4. Cardiac arrest: emergency 5. Hyperventilation: physiological support-breath from nose and mouth - do not give him o2..
Page 34 (9m 48s)
Is a process that involves removing whole blood from a donor or patient and then separating it into various components, including plasma, platelets and leukocytes. The desired component is collected, and the remainder of the blood is returned to the body. 2 type of Apheresis 1- Non therapeutic for donor Apheresis: ● Plateletpheresis 2- therapeutic Apheresis for patient: ● Plasmapheresis(for thrombotic thrombocytopenic purpura patients) in this disease the antibody attacks the platelet. The machine separates the bad RBCs and plasma and then returns a good plasma to the patient at the same time and by this way we discard the antibody that attack the platelet. ● Leuko-apheresis( cancer patient Leukemia) the WBC is very high. ● RBC exchange( sickle cell anemia when the patient make crises).
Page 35 (10m 17s)
Hematology……..
Page 36 (10m 23s)
WHAT IS HEMATOLOGY? Is the branch of biology, concerned with the study of blood, the blood- forming organs, and blood diseases. WHAT IS BLOOD? Is a specialized bodily fluid in animals that delivers necessary substances such as nutrients and oxygen to the cells and transports metabolic waste products away from those same cells. Functions of blood: 1. Gas transport - blood carries oxygen from lung to the tissues and carbon dioxide in reverse direction. 2. Transport of nutritional substances for all cells (glucose, amino acids, fatty acids, vitamins, ketone bodies, microelements etc.). Blood carries final products of metabolism (urea, uric acid, bilirubin, creatinin etc.) from tissues to kidney, where from they excreted with urine. 3. Regulation of different processes. Blood creates and carries local hormones (hormonoids) to the target organs. 4. Thermoregulation - heat change between tissues and blood. 5. Osmotic function - maintenance of the osmotic pressure in blood vessels. 6. Protective function - blood has antibodies and leucocytes, which perform phagocytosis. 7. Detoxification - blood enzymes can neutralize (split) different toxic substances..
Page 37 (11m 7s)
1. Color: Blood is red in color. Arterial blood is scarlet red because it contains more oxygen and venous blood is purple red because of more carbon dioxide. 2. Volume: Average volume of blood in a normal adult is 5 L. In a newborn baby, the volume is 450 ml. It increases during growth and reaches 5 L at the time of puberty. In females, it is slightly less and is about 4.5 L. It is about 8% of the body weight in a normal young healthy adult, weighing about 70 kg. 3. Reaction and pH: Blood is slightly alkaline and its pH in normal conditions is 7.4. 4. Specific gravity: ● Specific gravity of total blood : 1.052 to 1.061 ● Specific gravity blood cells : 1.092 to 1.101 ● Specific gravity of plasma : 1.022 to 1.026 5. Viscosity: Blood is five times more viscous than water. It is mainly due to red blood cells and plasma proteins..
Page 38 (11m 49s)
1. White Cell count (leukocyte count) 2. Platelet count 3. Red cell count, hemoglobin concentration and red cell indices. What Specimen? • Whole blood, un-centrifuged, anti-coagulated with EDTA (Purple or lavender cap). Cell Counts: • White cells, red cells (erythrocytes) and platelets are counted per unit volume of whole blood. • Unit volume: per cubic millimeter (mm3) which is the same as μL • WBC 4.0-10.0 x 103/cu mm • Platelets 150-450 x 103/cu mm • RBC 4.5-5.9 x 106/cu mm • Unit volume: per liter (SI units). • WBC 4.0-10.0 x 109/L • Platelets 150-450 x 109/L • RBC 4.5-5.9 x 1012/L.
Page 39 (12m 21s)
Abnormal White Blood Cells Neutrophils (AKA: PN4Ns, Polys, Segs) Neutrophils — Abnormalities in the neutrophil include..... 1. Greater than 5% bands 2. Hypersegmented nuclei (greater than 5 lobes) 3. Toxic granulation 4. Toxic vacuolization 5. Dohle bodies Normal granulation/ 6. Younger stages than the band vacuolization • •sepsis' 1 Band Alder—Reilly Hyper— segmented DNA DOhIe Bodies bad When do you see them in high numbers? Toxic granulation, vacuolization, & Dohle bodies are — Bacterial infections — Inflammation seen during bacterial infections, burns, cancer, and toxic or inflammatory states. Toxi.
Page 40 (12m 42s)
Hemoglobin & Red Cell Indices: 1. Hemoglobin 2. Hematocrit 3. Red cell count 4. Mean cell (corpuscular) volume or MCV 5. Mean cell hemoglobin concentration or MCHC 6. Mean cell hemoglobin content or MCH 7. Red cell distribution width or RDW.
Page 41 (12m 56s)
Hemoglobin concentration in grams/dL (grams per 100 mL) Normal: 12 -16 g/dL or 120 – 160 g/L Hemoglobin is converted to CYANMETHEMOGLOBIN which absorbs maximally at 540 nm • Hb plus KCN plus potassium ferricyanide + NaHCO3 • Heme iron (Fe2+) → Fe3+ • Methemoglobin binds with CN • Most current hematology analyzers have switched to a new, alternative method: sodium lauryl sulfate (SLS, SDS) binds to hemoglobin. • Sulfated derivative absorbs at 535 nm..
Page 42 (13m 14s)
Risks of High and Low Hemoglobin Levels Low hemoglobin levels are associated with: Elevated hemoglobin levels are associated with: kidney disease liver disease chronic lung disease dehydration anema (of several causes) verywell heart failure.
Page 43 (13m 24s)
the percentage of blood that is represented by the packed red cells.
Page 44 (13m 32s)
Plasma: - Water, proteins, nutrients, hormones, etc. Buffy coat: -..........................................-C - White blood cells, platelets Hematocrit: - Red blood cells Normal Blood: Q 37%-47% hematocrit 42%—52% hematocrit Anemia: Depressed hematocrit % Polycythemia: Elevated hematocrit %.
Page 45 (13m 45s)
Number of red blood cells per microliter of blood Normal range for Men: 4.5-6.0 for Women:4-5.
Page 46 (13m 55s)
Red cell volume in femtoliters or 10-15 liter Low MCV = Microcytic High MCV = Macrocytic Normal: 80-100.
Page 47 (14m 3s)
Approach to Anemia Low Mean Corpuscular Volume (<80 fL) • Iron Deficiency • Thalassemia • Lead Poisoning • Anemia of Chronic Disease Anemia Normal Mean Corpuscular Volume (80-100 fL) • Bleeding • Hemolysis • Marrow Failure • Anemia of Chronic Disease (e.g. Renal Disease, Liver Disease, Endocrinopathy, Chronic Inflammation, Chronic Infection) Mean Corpuscular Volume High Mean Corpuscular Volume (>100 fL) • B12 Deficiency • Folate Deficiency • Drugs • Reticulocytosis • Liver Disease • Hypothyroidism • Myelodysplasia 42.
Page 48 (14m 21s)
(Mean cell hemoglobin concentration (MCHC): Hemoglobin concentration of the packed red cells (minus plasma) Low MCHC: Hypo-chromic High MCHC Hyper-chromic Normal: 31-37 g/dL (of erythrocytes).
Page 49 (14m 33s)
1. 2. 3. 4. 5. 6. 7. 8. Seen In Thalassemia Cases Target Cells (Codocytes) Schistocytes (RBC Fragments) Helmet Celts (Bite Cells, Keratocytes) Teardrop Cells (Dacryocytes) Elliptocytes (Ovalocytes) Basophilic Stippling (Punctate Basophilia) Leptocytes (Hypochromic RBC's in Hgb H) Sickle Cells (Drepanocytes in HgbS/Thal) Left : Iron Deficiency B•Thalassemia Major (Cooley's) Suce: Mtp:/ um a c parum Gametocyte Banana Form) Beta Thalassemia Blood Smear Plasmodium fatéiparum Rings Elliptocytosis Cells Hereditary Spherocytosis Cells 0000 c, Plasmodium vivax Rings Plasmodium fatciparurn Schizont http:.
Page 50 (14m 53s)
Mean cell hemoglobin (MCH): Red cell hemoglobin content in Pico-grams or 10-12 grams Normal: 26 - 32 Pico-grams per red cell..