Page 1 (0s)
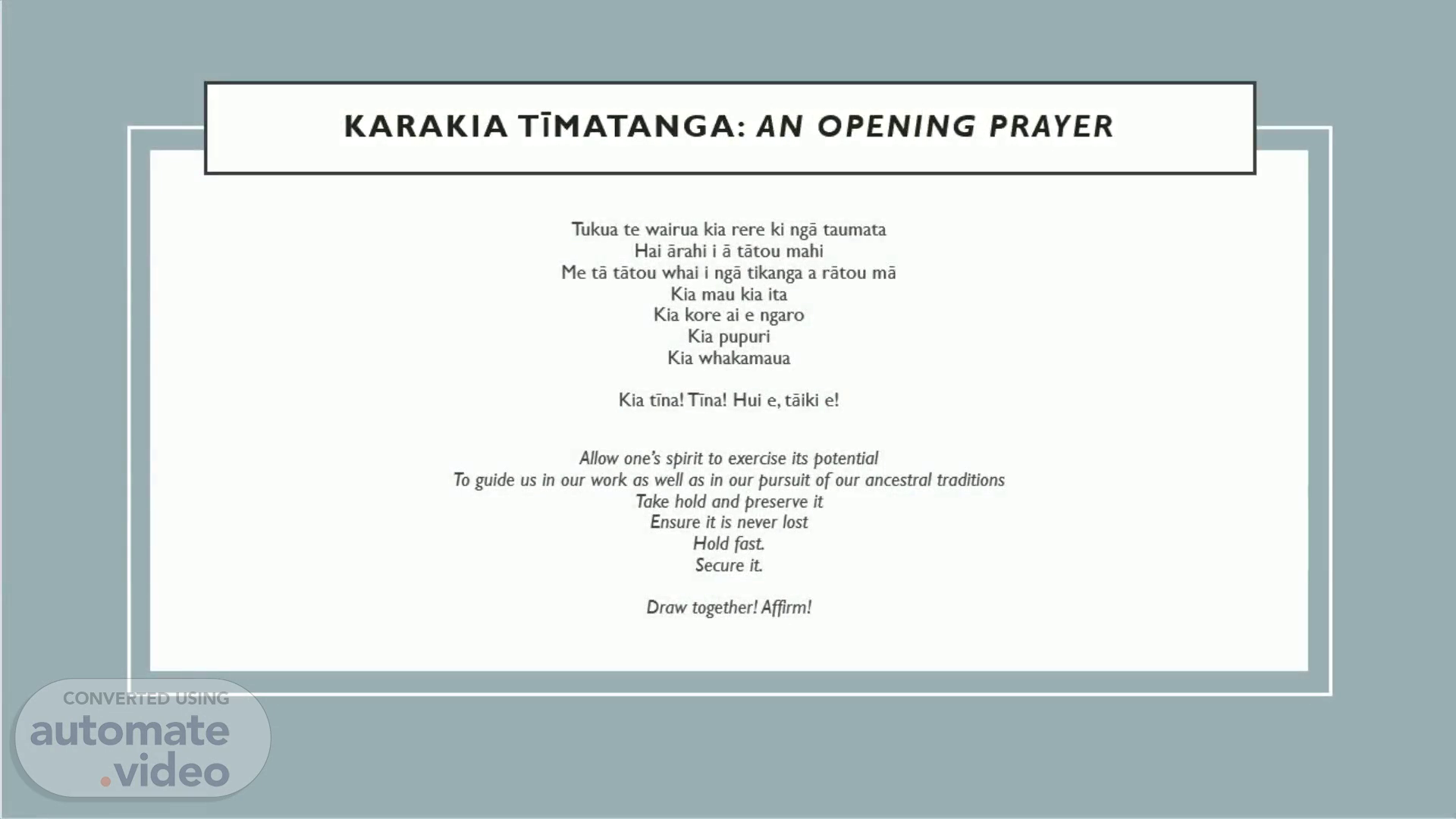
Karakia TĪMATAnga: AN OPENING prayer. Tukua te wairua kia rere ki ngā taumata Hai ārahi i ā tātou mahi Me tā tātou whai i ngā tikanga a rātou mā Kia mau kia ita Kia kore ai e ngaro Kia pupuri Kia whakamaua Kia tīna! Tīna! Hui e, tāiki e! Allow one’s spirit to exercise its potential To guide us in our work as well as in our pursuit of our ancestral traditions Take hold and preserve it Ensure it is never lost Hold fast. Secure it. Draw together! Affirm!.
Page 2 (23s)
1.mp3. OUTLINE. SUICIDE & MĀORI: A BRIEF HISTORY THE INEQUITY OF SUICIDE REDEFINING SUICIDE: A WHĀNAU MĀORI ISSUE SUICIDE THROUGH THE LENS OF TE TIRITI DRIVERS FOR EQUITY: WHAT HAS BEEN DONE SO FAR? DRIVERS FOR EQUITY: LOOKING FORWARD.
Page 3 (1m 23s)
2.mp3. SUICIDE & Māori: a brief history. Suicide was a part of pre-colonial Māori society, but mostly as a ritual act (Skegg et al., 1995) Official suicide statistics begin in 1889, delineated by ethnicity from 1931 (Hirini & Collings, 2005) Māori suicide rates doubled (females) and trebled (males) from 1957 – 1991 (Kingi et al., 2017) Data is unreliable due to colonised understandings of ethnic classification.
Page 4 (3m 42s)
3.mp3. THE INEQUITY OF SUICIDE. Indigenous suicide exists in a confluence of social, cultural, historical and economic factors (Lawson-Te Aho, 1997) Māori experience disparities in health outcomes across the board, including access to quality health care (Medical Council of New Zealand, 2019) Indigenous suicide is the end result of systematic negation, oppression and humiliation (Durie, 2001).
Page 5 (4m 39s)
4.mp3. THE INEQUITY OF SUICIDE. Suicide rates among Māori are almost double that of non-Māori (Ministry of Health, 2019b) Māori have less access to health determinants such as education, employment, secure housing and social support (Ministry of Social Development, 2006) Differences in socioeconomic status have accounted for over 20% of the difference in morbidity rate between Māori and non-Māori (Smith & Pearce, 1984) Māori experience more difficulty accessing healthcare (Sadler et al. 2004) Māori are less likely to receive quality care and more likely to experience adverse events (Davis et al., 2006) Māori almost twice as likely as non-Māori to avoid healthcare because of cost (Shoen & Doty, 2004) 34% of Māori reported experiencing discrimination within the healthcare system (Harris et al., 2006) Cultural wounding of colonisation: disconnection from identity, whenua and whanau as risk factors for suicide (Duran & Duran, 1995).
Page 6 (6m 17s)
5.mp3. REDEFINING SUICIDE: A WHāNAU MĀORI ISSUE. Suicide is shaped by spiritual, cultural and scientific beliefs (Durie, 2017) Conceptions of suicide are still entrenched in westernised understandings of the individual and disease models. These understandings don’t work for te ao Māori, which understands the individual as linked to whānau (Pitama et al., 2007) Kaupapa Māori sees whanaungatanga as primary source of resilience, strength and identity Indigenous suicide is not an individual problem, it is a collective responsibility.
Page 7 (7m 33s)
6.mp3. SUICIDE through the lens of TE TIRITI. Te Tiriti made explicit and implicit commitments to Māori health and protection (Kingi, 2007) A responsibility to equal rights and parity of outcomes An implicit obligation to equity, provision of resources and approaches that close inequitable healthcare gaps Tino rangatiratanga: the right to self-determination over health and wellbeing Control over Kaupapa Māori solutions to suicide Partnership and participation: whānau Māori included in decision-making and implementation of appropriate initiatives (Medical Council of New Zealand, 2019) A promise to allow Māori to define suicide and associated interventions on their own terms, and a commitment to resourcing this.
Page 8 (8m 33s)
7.mp3. DRIVERS FOR EQUITY: WHAT HAS BEEN DONE SO FAR?.
Page 9 (9m 15s)
8.mp3. DRIVERS FOR EQUITY: WHAT HAS BEEN DONE SO FAR?.
Page 10 (10m 0s)
9.mp3. DRIVERS FOR EQUITY: WHAT HAS BEEN DONE SO FAR?.
Page 11 (11m 6s)
10.mp3. DRIVERS FOR EQUITY: LOOKING FORWARD. Cultural competence vs. cultural safety (Pitama et al., 2007) A return of power to the patient – tino rangatiratanga (Dickson et al., 2022) Whānau have a key role in interventions and recovery Reducing economic and cultural barriers to treatment Accountability and self-reflection of biases at individual and organisational level Respecting Māori ways of knowing and being.
Page 12 (12m 21s)
11.mp3. DRIVERS FOR EQUITY: LOOKING FORWARD. Suicide is understood as a collective issue, inseparable from wider social and cultural inequities Suicide is a collective responsibility requiring whānau -based approaches Suicide exists in a hauora health matrix: spiritual, familial, historical, environmental.
Page 13 (13m 2s)
Karakia Whakamutunga: A closing prayer. Kia tau ngā manaakitanga a te mea ngaro Ki runga ki tēnā, ki tēnā o tātou Kia mahea te hua mākihikihi Kia toi te kupu, toi te mana, toi te aroha, toi te reo māori Kia tūturu, ka whakamaua Kia tīna! Tīna! Hui e, tāiki e! Let the strength and life force of our ancestors Be with each and every one of us Freeing our path from obstruction So that our words, spiritual power, love, and language are upheld; Permanently fixed, established and understood! Forward together!.
Page 14 (13m 28s)
REFERENCES. Byers, L. G. (2006). Depression, Discrimination, Trauma and American Indian Ethnic Identity. Dissertation Abstracts International: Humanities and Social Sciences, 67 , 717. Davis, P., Lay-Yee, R., Dyall, L., Briant, R., Sporle, A., Brunt, D., & Scott, A. (2006). Quality of hospital care for Māori patients in New Zealand: retrospective cross-sectional assessment. The Lancet, 367 , 1920-1925. Dickson, T., Wilkinson, T., Hegedus, E. J., & Gisselman, A. S. (2022). Transforming the Patient Experience: Moving Beyond Cultural Competence to Cultural Safety. Physical therapy . https://doi.org/10.1093/ptj/pzac034 Duran, B., & Duran, E. (1995). Native American Postcolonial Psychology . SUNY Press. Durie, M. (2001). Māuri Ora: The dynamics of Māori health . Oxford University Press. Durie, M. (2007). Whaiora. Māori health development (2nd ed.). Oxford University Press. Durie, M. (2017). Indigenous suicide: The Turamarama Declaration. Journal of Indigenous Wellbeing, 2 (2). Harris, R., & Robson, B. (2007). Hauora, Māori standards of health. a study of the years, 2000-2005 [eBook]. Te Rōpū Rangahau Hauora A Eru Pōmare. Harris, R., Tobias, M., Jeffreys, M., Waldegrave, K., Karlsen, S., & Nazroo, J. (2006). Effects of self reported racial discrimination and deprivation on Māori health and inequalities in New Zealand: cross-sectional study. The Lancet, 367 , 2005-2009. Health and Disability System Review. (2019). Interim report New Zealand health and disability system review: Hauora Manaaki Ki Aoteroa Whanui. NZ Government. Hirini, P., & Collings, S. (2005). Whakamomori, he whakaaro, he kōrero noa: A collection of contemporary views on Māori and suicide . Ministry of Health..
Page 15 (14m 34s)
REFERENCES. Kingi, T. K. (2007). The Treaty of Waitangi: a framework for Maori health development. New Zealand Journal of Occupational Therapy, 54 (1), 4-10. Kingi, T. K. R., Durie, M., Elder, H., Tapsell, R., Lawrence, M., & Bennett, S. (2017). Maea Te Toi Ora: Maori Health Transformations [Book]. Huia Publishers. Krieger, N., Rowley, D. I., Herman, A. A., Avery, B., & Phillips, M. T. (1993). Racism, sexism, and social class: implications for studies of health, disease, and wellbeing. American Journal of Preventive Medicine, 9 . Lawson-Te Aho, K. (1997). Kia Piki Te Ora O Te Taitamariki: A Review of the Evidence. Te Puni Kokiri (Ministry of Maori Development). Lawson-Te Aho, K. (2013). Whāia Te Mauriora - In Pursuit of Healing: Theorising connections between soul healing, tribal self-determination and Māori suicide prevention in Aotearoa/New Zealand [Unpublished Doctoral Thesis]. Victoria University. Lawson-Te Aho, K. (2014). The healing is in the pain: Revisiting and re-narrating trauma histories as a starting point for healing. Psychology and Developing Societies, 26 (2), 181-212. https://doi.org/10.1177/0971333614549139 Lorde, A. (1979). The Master’s Tools Will Never Dismantle the Master’s House. In C. Moraga & G. Anzaldúa (Eds.), This Bridge Called My Back: Writings from Radical Women of Color . Women of Color Press. Medical Council of New Zealand. (2019). He Ara Hauora Māori: A Pathway to Māori Health Equity . https://www.mcnz.org.nz/assets/standards/6c2ece58e8/He-Ara-Hauora-Maori-A-Pathway-to-Maori-Health-Equity.pdf . Medical Council of New Zealand. (2019). He Ara Hauora Māori: A Pathway to Māori Health Equity . https://www.mcnz.org.nz/assets/standards/6c2ece58e8/He-Ara-Hauora-Maori-A-Pathway-to-Maori-Health-Equity.pdf Ministry of Health. (2019a). Every Life Matters – He Tapu te Oranga o ia tangata: Suicide Prevention Strategy 2019–2029 and Suicide Prevention Action Plan 2019–2024 for Aotearoa New Zealand . Ministry of Health. Ministry of Health. (2019b). Wai 2575 Māori Health Trends Report . https://www.health.govt.nz/publication/wai-2575-maori-health-trends-report.
Page 16 (15m 40s)
REFERENCES. Ministry of Health. (2020). He Korowai Oranga . https://www.health.govt.nz/our-work/populations/maori-health/he-korowai-oranga Ministry of Social Development. (2006). The Social Report 2006: Indicators of social wellbeing in New Zealand . Ministry of Social Development. Pitama, S., Robertson, P., Cram, F., Gillies, M., Huria, T., & Dallas-Katoa, W. (2007). Meihana Model: A Clinical Assessment Framework. New Zealand Journal of Psychology, 36 (3), 118-125. Pitama, S. G., Bennett, S. T., Waitoki, W., Haitana, T. N., Valentine, H., Pahina, J., Taylor, J. E., Tassell-Matamua, N., Rowe, L., Beckert, L., Palmer, S. C., Huria, T. M., Lacey, C. J., & McLachlan, A. (2017). A proposed hauora Māori clinical guide for psychologists: Using the hui process and meihana model in clinical assessment and formulation. New Zealand Journal of Psychology, 46 (3). Sadler, L., Priest, P., Peters, J., Crengle, S., & Jackson, R. (2004). Cervical Cancer Audit report – screening of women with cervical cancer 2000– . Ministry of Health. Shoen, C., & Doty, M. (2004). Inequities in access to medical care in five countries: findings from the 2001 Commonwealth Fund International Policy Survey. Health Policy, 67 , 309-322. Skegg, K., Cox, B., & Broughton, J. (1995, 12//). Suicide among New Zealand Maori: is history repeating itself? Acta Psychiatrica Scandinavica, 92 (6), 453-459. Smith, A. H., & Pearce, N. E. (1984). Determinants of differences in mortality between New Zealand Maoris and non Maoris aged 15–64. New Zealand Medical Journal, 97 . Williams, A. D., Clark, T. C., & Lewycka, S. (2018, 2018-November-13). The Associations Between Cultural Identity and Mental Health Outcomes for Indigenous Māori Youth in New Zealand. Frontiers in Public Health, 6 . https://doi.org/10.3389/fpubh.2018.00319 Wilson, D., & Haretuku, R. (2015). Te Tiriti o Waitangi/Treaty of Waitangi 1840. In D. Wepa (Ed.), Cultural Safety in Aotearoa New Zealand (2 ed.). Cambridge University Press. https://doi.org/DOI : 10.1017/CBO9781316151136.