MedCom_TraumaticBrainInjury_1E_9789390553983_15,2x22,9_(6x9')SC_3Seiten_k8.indd part 3
Scene 1 (0s)
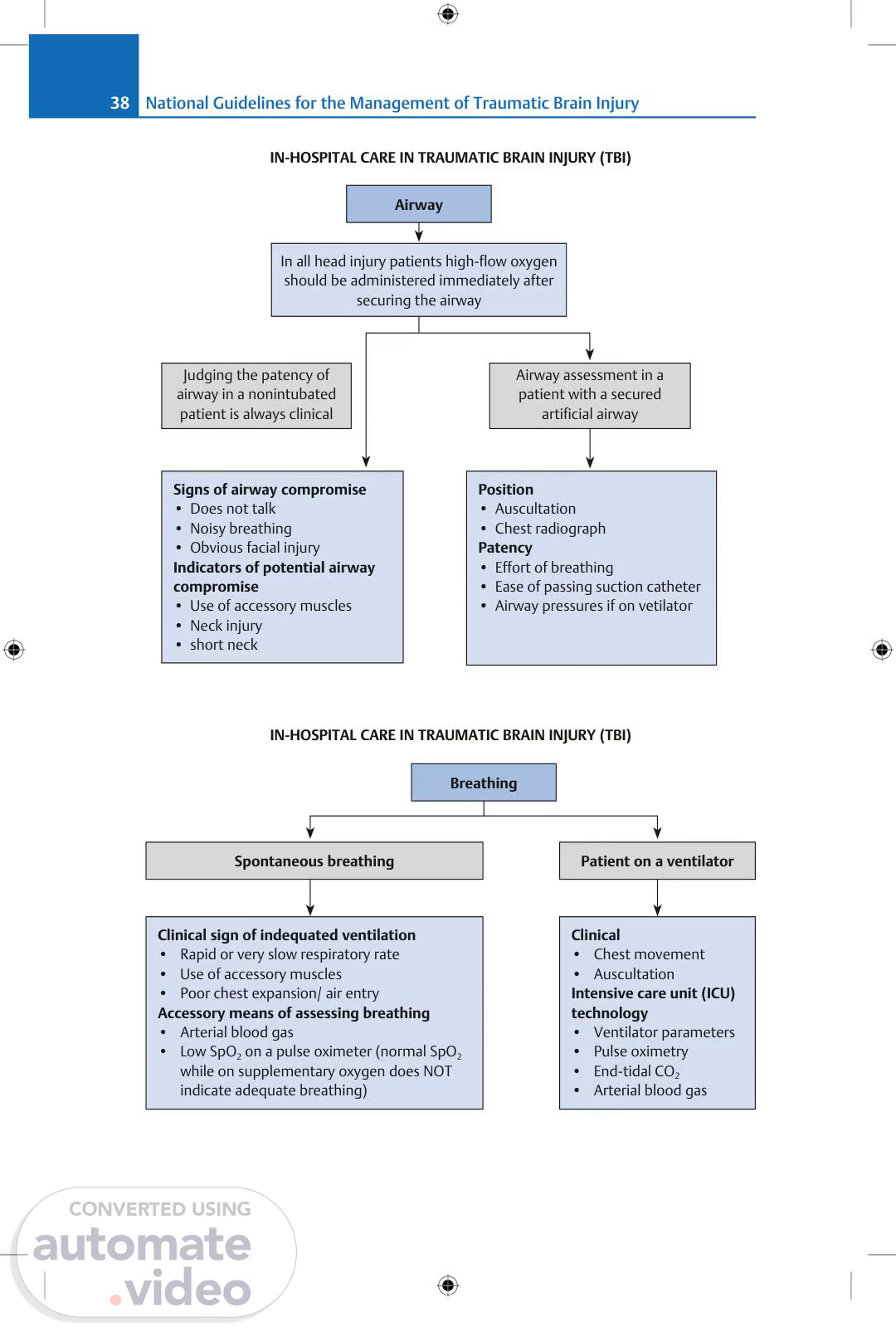
[Audio] National Guidelines for the Management of Traumatic Brain Injury 38 IN-HOSPITAL CARE IN TRAUMATIC BRAIN INJURY (TBI) Airway In all head injury patients high-flow oxygen should be administered immediately after securing the airway Judging the patency of airway in a nonintubated patient is always clinical Airway assessment in a patient with a secured artificial airway Position Auscultation Chest radiograph Patency Effort of breathing Ease of passing suction catheter Airway pressures if on vetilator Signs of airway compromise Does not talk Noisy breathing Obvious facial injury Indicators of potential airway compromise Use of accessory muscles Neck injury short neck IN-HOSPITAL CARE IN TRAUMATIC BRAIN INJURY (TBI) Breathing Spontaneous breathing Patient on a ventilator Clinical sign of indequated ventilation Rapid or very slow respiratory rate Use of accessory muscles Poor chest expansion/ air entry Accessory means of assessing breathing Arterial blood gas Low SpO2 on a pulse oximeter (normal SpO2 while on supplementary oxygen does NOT indicate adequate breathing) Clinical Chest movement Auscultation Intensive care unit (ICU) technology Ventilator parameters Pulse oximetry End-tidal CO2 Arterial blood gas.
Scene 2 (1m 31s)
[Audio] Summary and Conclusions 39 IN-HOSPITAL CARE IN TRAUMATIC BRAIN INJURY (TBI) Blood pressure Emergency room signs of impaired circulation Pulse—trchycardia, poor valume Blood pressure Capillary refill > 2 seconds, cold extremities Auscultation for pneumothorax or tamponade Monitored area (in emergency room [ER] or high care area) Heart rate Noninvasive blood pressure Invasive blood pressure—if significant Instability present or on vasoactive drugs IN-HOSPITAL CARE IN TRAUMATIC BRAIN INJURY (TBI) Intervention Airway Answers Talk to the patient Airway is secure If he does not speak Jaw thrust Remove foreign body (FB) Perform oral suction Noisy breathing/significant blood in oral cavity Insert an oral airway If a definitive airway was not initially necessary frequent reassessment of the airway is mandatory If not available Definitive airway Turn patient semiprone If not possible a cricothyroidotomy Endotracheal intubation/ laryngeal mask airway is the primary option Connect high-flow oxygen after securing airway.
Scene 3 (2m 47s)
[Audio] National Guidelines for the Management of Traumatic Brain Injury 40 IN-HOSPITAL CARE IN TRAUMATIC BRAIN INJURY (TBI) Intervention Breathing Inadequate Definitive airway (unless the reason is rapidly correctable such as a tension pneumothorax) Endotracheal tube* Continue manual assistance and correct cause of impaired breathing Connect to ventilator and refer to higher center *Requires sedation and often muscle relaxants, following which breathing has to be assisted—manually or (where available) with a ventilator. Supplementary oxygen Avoid hyperventilation (common with manual ventilation) IN-HOSPITAL CARE IN TRAUMATIC BRAIN INJURY (TBI) Intervention Blood pressure Low blood pressure (BP)/patient has tachycardia with borderline BP Continue crystalloids rapidly and monitor pulse and blood pressure After > 1 lt—RL preferred O– blood BP does not respond Large caliber peripheral lines in both antecubital fossae (dextrosefree crystalloids @ maximum) Not ready Blood cross match Vasoactive drugs— to raise BP Controlled No facilities Refer urgently to a higher center while continuing rapid infusion of crystalloids en route Unstable BP Control hemorrhage External Pressure Abdomen—urgent surgical consultation Pelvis—apply binder Femur—splint Surgical control of hemorrhage.
Scene 4 (4m 22s)
[Audio] Summary and Conclusions 41 Head Injury—Gasgow Coma Scale (GCS) Score in normal adults is 15 A. Eye opening Spontaneously 4 To speech 3 To pain 2 None 1 C. Best motor response Obeys commands 6 Localization to pain 5 Withdrawal to pain 4 Spastic flexion to pain 3 Extension to pain 2 None 1 B. Best verbal response Orientated 5 Confused 4 Inappropr words 3 Incompr sounds 2 None 1 Algorithm for Mx of mild head injury History G/E Neurological examination Skull X-Ray Cervical spine X-Ray Blood Alcohol levels Computed tomography (CT) head—ideally in all but completely asymptomatic patients Admit Discharge Does not meet criterion for admission Discuss need to return if problem Amnesia H/o loss of consciousness (LOC) Deteriorating conciousness Moderate-to-severe headache Alcohol/drug intoxication Skull fracture Cerebrospinal fluid (CSF) leak Significant ass injuries Abnormal CT scan.
Scene 5 (5m 42s)
[Audio] National Guidelines for the Management of Traumatic Brain Injury 42 Algorithm for Mx of moderate head injury Initial w/u Computed tomography (CT) scan in all cases ADMIT even if CT is normal Frequent neurological examinations Follow up (FU) CT Scan if deteriorates/before discharge If pt improves (90%) If pt deteriorates (10%) Discharge when stable Repeat CT Scan Manage as per severe HI Algorithm for Mx of severe head injury History Rescuscitaion—airway, breathing, and circulation (ABC) Catheters X-Rays—Cx/Chest/Skull/Abdomen/ Pelvis/Extremities G/E Emergency measures for ass injuries: Tracheostomy Chest tubes Neck stabilization Abdominal paracentesis Neurological examination.
Scene 6 (6m 50s)
[Audio] Summary and Conclusions 43 Algorithm for Mx of severe head injury Intubate, Sedate, Resuscitate Computed tomography (CT) Scan Not available Refer to higher level if < 2 hours Diffuse lesion Surgical lesion Operation theater (OT) Intensive care unit (ICU) Monitor intracranial pressure (ICP) Elevate Head end Sedate Maintain Pao2 100 mmHg Maintain PaCo2 30–32 mmHg ICP still high Treat ICP Monitor ICP ICP<20 ICP<20 Check PaO2, PacO2 Head/Neck position Treat pain, Fever Recalibrate ICP system Repeat CT No surgical mass lesion Surgical mass lesion Craniotomy Mannitol/Loo Diuretics Hyperventilate Barbiturate Coma Decompressive craniotomy (DC) Lobectomy.
Scene 7 (7m 11s)
[Audio] National Guidelines for the Management of Traumatic Brain Injury 44 IN-HOSPITAL CARE IN TRAUMATIC BRAIN INJURY (TBI) Criteria for performing a computed tomography (CT) head scan Adults Children Glasgow Coma Scale (GCS) < 13 on initial assessment in emergency department (ED) GCS <15 at 2 hours after the injury in ED Suspected open/depressed skull fracture Any sign of basal skull fracture (hemotympanum, "panda" eyes, cerebrospinal fluid leakage from the ear or nose, Battle sign) Posttraumatic seizure Focal neurological deficit > 1 episode of vomiting Posttraumatic seizure but no history of epilepsy GCS < 14, or for children < 1 year -GCS (pediatric) < 15 At 2 hours after the injury, GCS < 15 Suspected open/depressed skull fracture or tense fontanelle Any sign of basal skull fracture (hemotympanum, "panda" eyes, cerebrospinal fluid leakage from the ear or nose, Battle sign) Focal neurological deficit Loss of consciousness > 5 minutes (witnessed) Abnormal drowsiness or irritability 3/> e/o vomiting Dangerous mechanism of injury (high-speed road traffic accident either as pedestrian, cyclist, or vehicle occupant, fall from a height of > 3 m, highspeed injury from a projectile or other object) Amnesia (antegrade/retrograde) > 5 minutes.
Scene 8 (8m 4s)
[Audio] The need for the development of guidelines for the management of traumatic brain injury (TBI) has long been a matter of concern to the treating medical personnel, and its importance has been recognized ever since improvements in TBI outcomes have been reported after the adoption of similar guidelines by the more developed nations across the globe. The Neurotrauma Society of India (NTSI) in collaboration with the Neurological Society of India (NSI) took up the mammoth responsibility of bringing forth these India-centric guide- lines in a concise and comprehensive manner. A logical effort has been made to make these guidelines as practical as possible, depending upon the resources available at the treating hospital, rather than keeping them "ideal" but impractical to follow. These guidelines are expected to bring about an enormous change in the management of TBI across the country, especially if followed by the treating doctors, thereby improving the outcomes of TBI. —Neurotrauma Society of India (NTSI) An award-winning international medical and scientific publisher, Thieme has demonstrated its commitment to the highest standard of quality in the state-of-the-art content and presentation of all its products. Founded in 1886, the Thieme name has become synonymous with high quality and excellence in online and print publishing. ISBN 978-93-90553-98-3 9 7 8 9 3 9 0 5 5 3 9 8 3 www.thieme.in MedCom_TraumaticBrainInjury_1E_9789390553983_15,2x22,9_(6x9')SC_3Seiten_k5.indd 1,3 MedCom_TraumaticBrainInjury_1E_9789390553983_15,2x22,9_(6x9')SC_3Seiten_k5.indd 1,3.