Retention, stability and support
Scene 1 (0s)
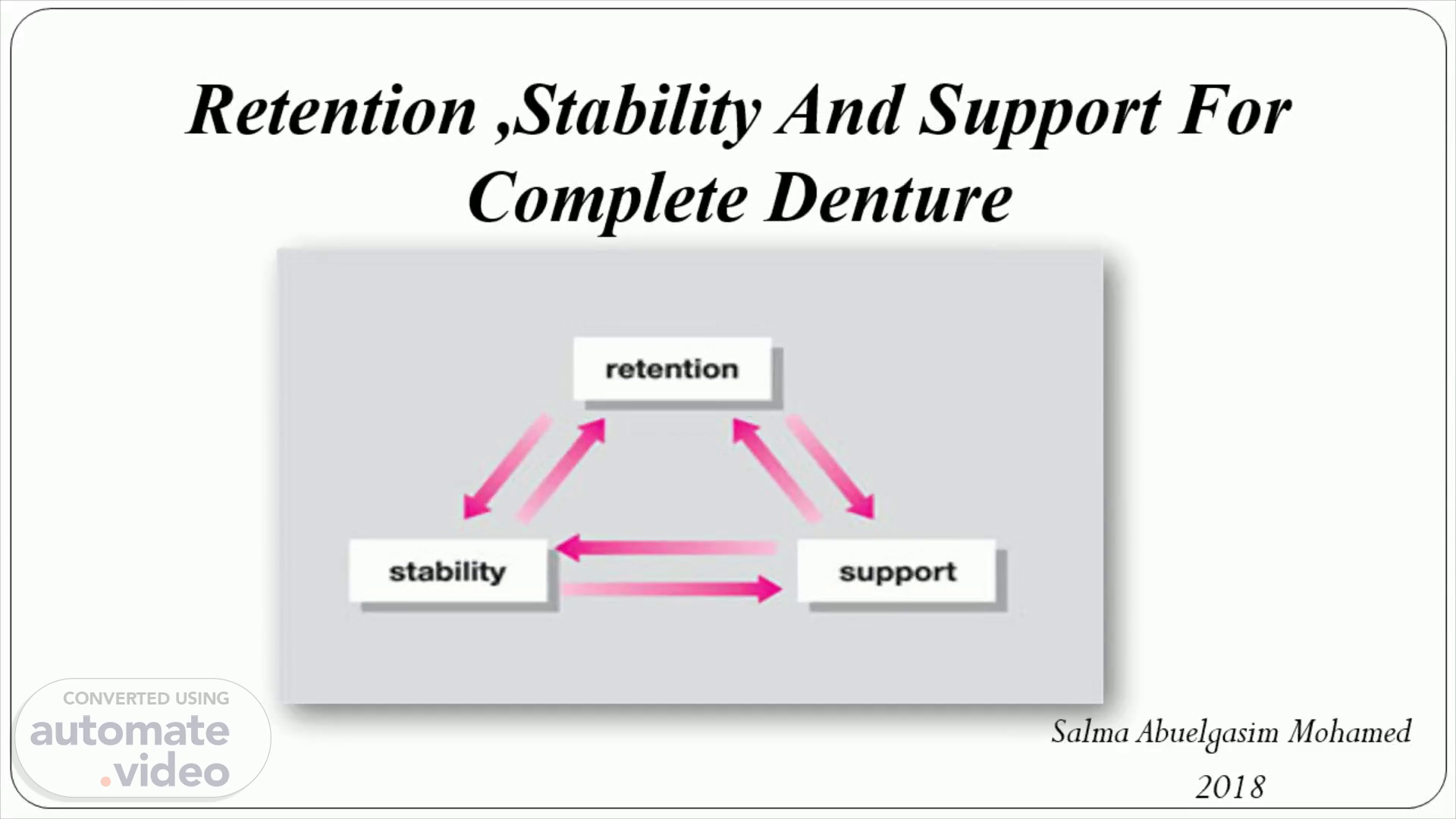
retention stability support. Retention ,Stability And Support For Complete Denture.
Scene 2 (32s)
Psychological Comfort. Physiological Comfort. Longevity.
Scene 3 (1m 40s)
Objectives. By the end of this session the participants should be able to Define retention ,stability and support Determined the factors affecting.
Scene 4 (2m 3s)
RETENTION Definitions The factors affecting the retention of complete dentures STABILITY Definitions Factors affecting the Denture Stability SUPPORT Definitions Type of support Areas of support factors affecting the Denture support.
Scene 5 (2m 40s)
Preservation of remaining alveolar ridges Support Stability Retention Esthetics.
Scene 6 (3m 13s)
To provide adequate masticatory function To restore natural appearance To restore normal speech Comfort and preservation of supporting structure.
Scene 7 (4m 15s)
1- It is the resistance of a denture to vertical movement away from the tissues foundation specially in a vertical direction 2- That quality inherent in the prosthesis acting to resist the forces of dislodgement along the path of insertion..
Scene 8 (5m 36s)
BOUCHER Described retention as the most spectacular yet probably the least important of all complete denture objectives. This property may indeed be least important, it provides psychological comfort to patient..
Scene 9 (5m 48s)
The act of chewing of food . Adhesive nature of certain food. Gravity(in case of the upper denture). Surrounding musculature (cheeks ,tongue , soft palate) Prematurities in the occlusion when the dentures contact without food being present or during parafunctional activity ..
Scene 10 (8m 36s)
1. Physical factors . 2. Anatomical factors. 3. Physiological factors. 4. Mechanical factors. 5. Biological factors ..
Scene 11 (9m 3s)
Principles Of Complete Denture Retention. Physical.
Scene 12 (10m 44s)
1. Physical factors. Adhesion Cohesion Surface tension Atmospheric pressure (peripheral seal) Gravity.
Scene 13 (11m 6s)
Adhesion. The apparent force of attraction existing between dissimilar bodies in close contact Is the physical attraction of unlike molecules It act when saliva sticks to the denture base and the mucous membrane of the basal seat.
Scene 14 (11m 55s)
Effectiveness of adhesion depends on:-. Close adaptation of the denture base to the supporting tissue. The type of the saliva. Shape and surface of the denture bearing area . The direction of the displacing forces..
Scene 15 (13m 56s)
https tse4 mm bing net th id OIP QgZAsPJnyYMOWAJKFJtTwCVDw pid 15 1 P 0 w 300 h 300.
Scene 16 (14m 32s)
Mucosa. Saliva. Adhesion Cohesion Adhesion. Denture.
Scene 17 (15m 32s)
• Resistance to separation by the film of liquid between the denture base & the supporting tissues . • Dependent on the ability of the fluid to wet the rigid surrounding material.
Scene 18 (16m 49s)
ADHESION Thin film of Saliva between the denture bearing area, and the denture base. COHESION Attraction of like molecules of saliva aiding in retention INTERFACIAL SURFACE TENSION Thin film of saliva resisting displacing forces, and little liquid-air interface.
Scene 19 (17m 50s)
Factor affects the atmospheric pressure:- Perfect peripheral seal. Proper border molding. Selective pressure technique..
Scene 20 (20m 12s)
The peripheral seal is the positive contact of the entire perimeter of the denture base to the resilient tissues that outline the basal seat This includes the posterior palatal seal as well as all labial, buccal and lingual vestibules.
Scene 21 (21m 4s)
Gravity. Gravity acts as retentive forces for the mandibular denture and a displaced for the maxillary denture when patient is in upright posture..
Scene 24 (22m 15s)
Shape of the ridge Edentulous ridges are firm and regular and covered by firmly attached , dense mucoperiostem should be vertical ,parallel sides produces the best resistance to un stabilizing forces.
Scene 25 (22m 50s)
Image007. Excellent prognosis. Image016. Good prognosis.
Scene 26 (25m 10s)
2 . Undercuts The contour of a cross-sectional portion of a residual ridge or dental arch that prevents the insertion of a dental Prosthesis Any irregularity in the wall of a prepared tooth that prevents the withdrawal or seating of a wax pattern or casting.
Scene 27 (26m 13s)
l}: Sidc.
Scene 28 (27m 30s)
3.Anatomy of the border tissues The anatomy of the border tissues should be such that it is possible to develop a good denture flange ,the periphery of which can lie in contact with displaceable and elastic tissue.
Scene 31 (28m 4s)
2.Saliva:. . 3.Physiological factors.
Scene 32 (28m 43s)
Neuromuscular control Refer to the functional forces exerted by the musculature of the patient that can affect denture retention.
Scene 34 (29m 40s)
The bilateral, simultaneous, anterior, and posterior occlusal contact of teeth in centric and eccentric positions.
Scene 35 (31m 51s)
Intimate tissues contact ; obtainable by accurate impression Peripheral seale. posterior palatal seal is most important in maintaining seal on the maxillary denture lingual flange area.
Scene 36 (33m 3s)
6.Aids to retention. Springs Magnets Denture adhesive micro valves.
Scene 37 (34m 8s)
Retention test.
Scene 39 (34m 44s)
Stability. Definition: The quality of a removable dental prosthesis to be firm, steady, or constant, to resist displacement by functional horizontal or rotational stresses Resistance to horizontal movement and the forces that tend to alter the relationship between the denture base and its surrounding foundation.
Scene 40 (35m 51s)
Retention Residual ridge anatomy Residual ridge relationships Parallelism of the ridges Form and contour of the polished surface Stability of the denture base material Arch arrangement Occlusal plane Occlusal harmony Neuromuscular control.
Scene 41 (37m 44s)
Stability test.
Scene 43 (38m 15s)
Support. The resistance to vertical movement or displacement of the denture towards the denture bearing area . The foundation area on which a dental prosthesis rests..
Scene 44 (39m 5s)
Complete denture support. The resistance to vertical movement of the denture base toward the ridge.
Scene 45 (40m 36s)
Primary stress- bearing areas Secondary stress- bearing areas Relief areas Valves seal areas.
Scene 46 (41m 17s)
Secondary stress – bearing areas. Aras which by their histological make-up or by the nature of their inclined planes , resist lateral forces of occlusion and can also aid in resistance to vertical forces of occlusion.
Scene 47 (42m 46s)
Valve seal areas. Area are those soft tissue border areas which the periphery of the denture must contact in order for the factors of retention to be effective Divided.
Scene 48 (45m 13s)
Relief Areas Posterior Palatal Seal Valve Seal Areas Primary Stress- bearing Areas Secondary Stress- bearing Areas Fig. 8.6 Classification of the denture-bearing tissues (Denture Foundation)..
Scene 49 (45m 23s)
Areas of support:. Anatomy of edentulous maxilla Primary stress bearing area: Horizontal portion of had palate Secondary stress bearing area: ridge crest (2). Non stress bearing area ridge slopes wc—.
Scene 50 (45m 35s)
Anatomy of edentulous Mandible Primary stress bearing area: buccal shelf & retromaolar pad Secondary stress bearing area Residual ridge & genial tubercles (2) Non stress bearing area Labial and lingual inclines.