Scene 1 (0s)
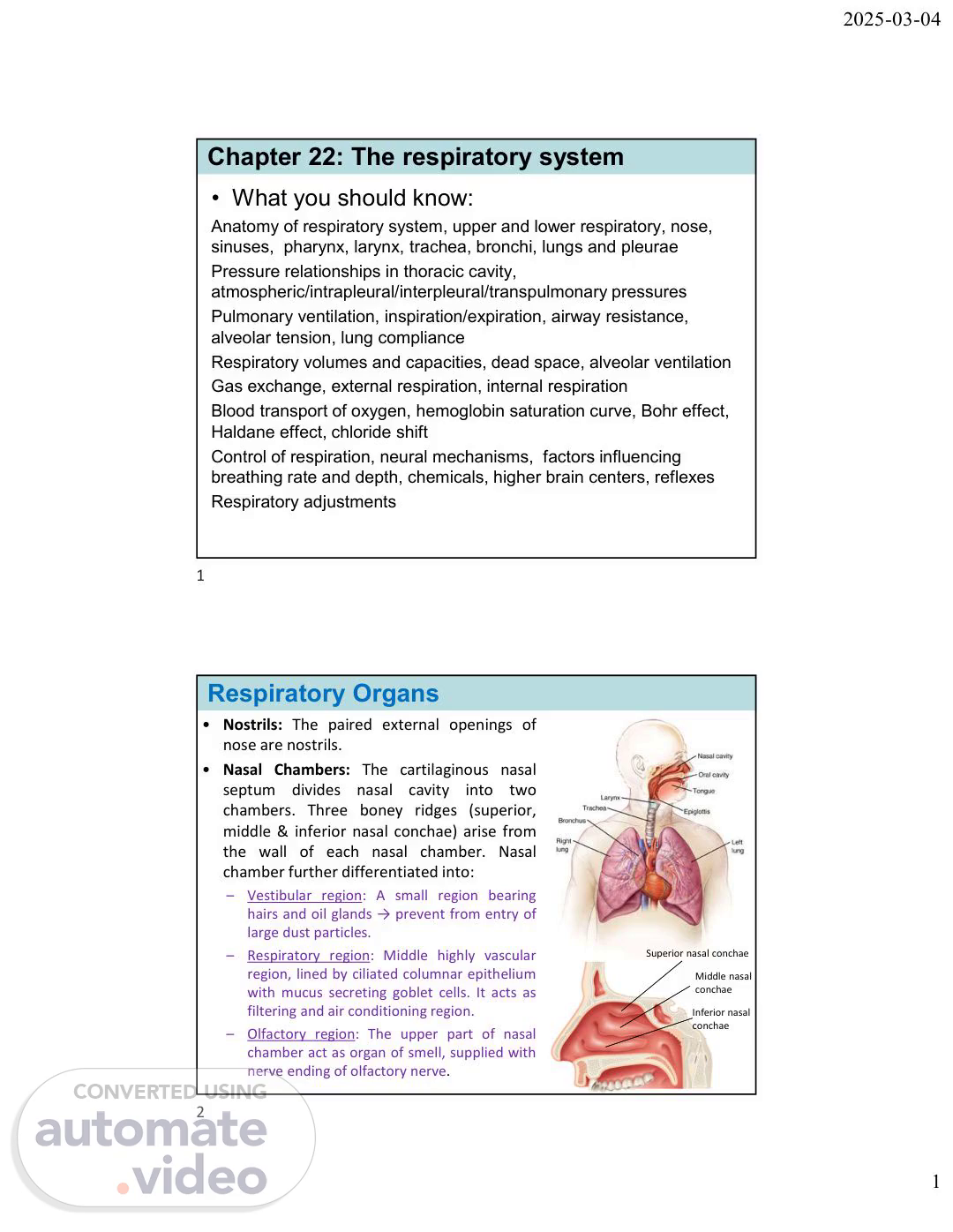
[Audio] 2025-03-04 Chapter 22: The respiratory system What you should know: Anatomy of respiratory system, upper and lower respiratory, nose, sinuses, pharynx, larynx, trachea, bronchi, lungs and pleurae Pressure relationships in thoracic cavity, atmospheric/intrapleural/interpleural/transpulmonary pressures Pulmonary ventilation, inspiration/expiration, airway resistance, alveolar tension, lung compliance Respiratory volumes and capacities, dead space, alveolar ventilation Gas exchange, external respiration, internal respiration Blood transport of oxygen, hemoglobin saturation curve, Bohr effect, Haldane effect, chloride shift Control of respiration, neural mechanisms, factors influencing breathing rate and depth, chemicals, higher brain centers, reflexes Respiratory adjustments 1 Respiratory Organs Nostrils: The paired external openings of nose are nostrils. Nasal Chambers: The cartilaginous nasal septum divides nasal cavity into two chambers. Three boney ridges (superior, middle & inferior nasal conchae) arise from the wall of each nasal chamber. Nasal chamber further differentiated into: – Vestibular region: A small region bearing hairs and oil glands → prevent from entry of large dust particles. Superior nasal conchae Middle nasal conchae – Respiratory region: Middle highly vascular region, lined by ciliated columnar epithelium with mucus secreting goblet cells. It acts as filtering and air conditioning region. Inferior nasal conchae – Olfactory region: The upper part of nasal chamber act as organ of smell, supplied with nerve ending of olfactory nerve. 2 1.
Scene 2 (1m 50s)
[Audio] 2025-03-04 Respiratory Organs Sinuses: Air filled cavities located within the bones of skull and face. Lined by mucous membranes and connected to the nasal passages. – Types: Frontal, Maxillary, Ethmoid, and Sphenoid sinuses. – Function: humidifying and warming the air, lightening the skull, mucus secretion to trap and expel foreign particles, bacteria, and viruses. Internal Nares: these are the posterior opening of nasal chambers lead into the nasopharynx. Pharynx: It is the passage for both air & food; and comprises of three parts: – Nasopharynx passage way for air only – Oropharynx passage way for both air and food – Hypopharynx (Laryngopharynx) passage way for both air and food 3 Respiratory Organs Larynx (Voice box): A small swollen part of respiratory tract lies at the level of 3rd, 4th, & 5th cervical vertebrae. Size: male>female. Also called as Adam’s apple. It consists of following structures: – Glottis: A narrow slit like opening of larynx. – Cartilages: Nine pieces of cartilages are: → epiglottis (1), thyroid cartilage (1), cricoid cartilage (2), arytenoids cartilages (2), corniculate cartilages (2), and cuneiform cartilages (2) – Hyoid bone: Lies just below the tongue and above the larynx. – Thyrohyoid membrane, ligaments and muscles: Provide support to different cartilages of the larynx and help in movement of larynx. – Vocal cords: Two folds of mucus membrane, extended into the lumen. Made of yellow elastic tissue covered by epithelium. Among the two folds, upper vocal cords → false vocal cord and lower vocal cords → true vocal cords (as it produces sound due to its vibration). 4 2.
Scene 3 (3m 41s)
[Audio] 2025-03-04 Respiratory Organs Trachea (Windpipe): Long tubular structure (about 12 centimeters long and 2.5 centimeters wide), bearing 16 to 20 incomplete rings made of C shaped hyaline cartilage. Cartilage help in supporting the tracheal wall, prevent from its twisting and collapse, also assist in the process of swallowing. Trachea is lined by ciliated epithelium bearing secretary cells. Mucus traps the dust particles, and the ciliary motion expels it out by coughing. Trachea divides into a pair of bronchi (primary bronchi) also having cartilaginous rings 5 Respiratory Organs Lungs (Pulmones): A pair of lungs lies inside the thoracic cavity, one on either side of the heart. Lungs are soft, spongy, and elastic organ. Left lung has two lobes (superior and inferior) and right lung has three lobes (superior, middle and inferior). It is externally covered by double layered pleura (outer parietal and inner visceral pleura) and the space between them (pleural cavity) is filled with pleural fluid. – The pleural fluid lubricates the pleura and allows no friction during breathing. – Several branches of bronchi (primary bronchi → secondary bronchi → tertiary bronchi → bronchioles → → → respiratory bronchioles → alveolar duct → alveoli). – Alveoli are small sac like structures of lungs that lined with single layer of squamous epithelium, which are highly vascular, where the gaseous exchange takes place by diffusion. 6 3.
Scene 4 (5m 20s)
[Audio] 2025-03-04 Respiratory Organs 7 Respiratory Organs Respiratory Muscles: Two types of respiratory muscles that help during inspiration and expiration. – Intercostal Muscles: 11 pairs of intercostal muscles found in between two ribs. Three major layers: external, internal and innermost intercostal muscles, and has capability of contraction and relaxation. – Diaphragm: Dome shaped fibromuscular structure that separate thoracic cavity from abdominal cavity. It also has capability of contraction and relaxation. 8 4.
Scene 5 (6m 2s)
[Audio] 2025-03-04 Respiration Major functions of respiratory system: supply body with O2 for cellular respiration and dispose of C-O-2--, a waste product of cellular respiration Respiratory and circulatory system are closely coupled Also functions in olfaction and speech Respiratory Respiration involves four processes 1. Pulmonary ventilation (breathing): movement of air into and out of lungs system 2. External respiration: exchange of O2 and C-O-2 between lungs and blood 3. Transport of O2 and C-O-2 in blood Circulatory system 4. Internal respiration: exchange of O2 and C-O-2 between systemic blood vessels and tissues 9 Respiratory epithelium 10 5.
Scene 6 (6m 52s)
[Audio] 2025-03-04 Respiratory membrane – Blood air barrier that consists of alveolar and capillary walls and their fused basement membranes, very thin (~0.5 m) to allow gas exchange by simple diffusion – Alveolar walls consist of: – Single layer of squamous epithelium (type I alveolar cells) – Sparse cuboidal type 2 alveolar cells make surfactant and antimicrobial proteins – Other features of alveoli: 1. Surrounded by fine elastic fibers and pulmonary capillaries 2. Alveolar pores connect adjacent alveoli equalizing air pressure and providing detours in case of blockages 3. Alveolar macrophages keep alveolar surfaces free of pathogens: 2 million (dead cells, pathogens & macrophages)/hour carried by cilia to throat and swallowed 11 Respiratory Physiology: Mechanics of Breathing Pulmonary ventilation consists of two phases – Inspiration: gases flow into lungs – Expiration: gases exit lungs © 2016 Pearson Education, Inc. 12 6.
Scene 7 (8m 7s)
[Audio] 2025-03-04 Atmospheric pressure (Patm) 0 millimeters Hg (760 millimeters Hg) Parietal pleura Thoracic wall Visceral pleura Pleural cavity Transpulmonary pressure 4 millimeters Hg (the difference between 0 millimeters Hg and 4 millimeters Hg) 4 0 Intrapleural pressure (Pip) 4 millimeters Hg (756 millimeters Hg) Lung Diaphragm Intrapulmonary pressure (Ppul) 0 millimeters Hg (760 millimeters Hg) © 2016 Pearson Education, Inc. 13 Pressure Relationships in the Thoracic Cavity Atmospheric pressure (Patm) is pressure exerted by air on body – 760 millimeters Hg at sea level = 1 atmosphere All respiratory pressures are relative to Patm – Negative respiratory pressure: less than Patm – Positive respiratory pressure: greater than Patm – Zero respiratory pressure: equal to Patm Intrapulmonary pressure (Ppul) or intra alveolar pressure is pressure in alveoli, it fluctuates with breathing and eventually equalizes with Patm Intrapleural pressure (Pip): is pressure in pleural cavity that fluctuates with breathing – Always negative (<Patm and <Ppul), ~ 4 millimeters Hg less than Ppul – Fluid level kept at a minimum and excess fluid picked up by lymphatic system, if fluid accumulates, positive Pip pressure develops and lung collapses 14 7.
Scene 8 (9m 30s)
[Audio] 2025-03-04 Pressure Relationships in the Thoracic Cavity Intrapleural pressure (Pip): – Two inward forces promote lung collapse 1. Lungs’ elasticity and natural tendency to recoil 2. Surface tension of alveolar fluid pulls on alveoli to try to reduce alveolar size – One outward force tends to enlarge lungs Elasticity of chest wall pulls thorax outward – Negative Pip is affected by these opposing forces but is maintained by strong adhesive force between parietal and visceral pleurae Transpulmonary pressure Pressure that keeps lung spaces open, keeps lungs from collapsing = (Ppul Pip) Greater transpulmonary pressure, the larger the lungs Lungs will collapse if: Pip = Ppul or Pip = Patm Negative Pip must be maintained to keep lungs inflated 15 Pulmonary Ventilation Consists of inspiration and expiration Mechanical process that depends on volume changes in thoracic cavity: volume changes lead to pressure changes pressure changes lead to flow of gases to equalize pressure Boyle’s law: relationship between pressure and volume of a gas – Gases always fill the container they are in If amount of gas is the same and container size is reduced, pressure will increase – So pressure (P) varies inversely with volume (V) – Mathematically: P1V1 = P2V2 16 8.
Scene 9 (10m 54s)
[Audio] 2025-03-04 Inspiration Inspiration is an active process involving inspiratory muscles (diaphragm and external intercostals) Action of the diaphragm: dome shaped diaphragm contracts, moves inferiorly and flattens out: increase in thoracic volume Action of intercostal muscles: external intercostals contract, rib cage is lifted up and out: increase in thoracic volume – As thoracic cavity volume increases, lungs stretch with thoracic cage: intrapulmonary pressure drop by 1 millimeters Hg: Ppul < Patm Difference between atmospheric and intrapulmonary pressure cause air flows in lungs, down pressure gradient, until Ppul = Patm – During same period, Pip lowers to ~ 6 millimeters Hg less than Patm Forced (deep) inspirations occur during exercise increase thoracic volume and increase pressure gradient: – accessory muscles are activated: scalenes, pectoralis minor and sternocleidomastoid – Erector spinae muscles help to straighten thoracic curvature 17 © 2016 Pearson Education, Inc. 18 9.
Scene 10 (11m 28s)
[Audio] 2025-03-04 Expiration – Quiet expiration normally is passive process Inspiratory muscles relax, thoracic cavity volume decreases, and lungs recoil Volume decrease causes intrapulmonary pressure (Ppul) to increase by plus 1 millimeters Hg Ppul > Patm so air flows out of lungs down its pressure gradient until Ppul = Patm – Forced expiration is an active process that uses oblique and transverse abdominal muscles, as well as internal intercostal muscles 19 © 2016 Pearson Education, Inc. 20 10.
Scene 11 (12m 9s)
[Audio] 2025-03-04 Changes in intrapulmonary and intrapleural pressures during inspiration and expiration. Inspiration Expiration 2 Intrapulmonary pressure 0 Intrapulmonary pressure. Pressure inside lung decreases as lung volume increases during inspiration; pressure increases during expiration. 2 Transpulmonary pressure 4 6 Intrapleural pressure 8 Pressure relative to atmospheric pressure (mm Hg) Intrapleural pressure. Pleural cavity pressure becomes more negative as chest wall expands during inspiration. Returns to initial value as chest wall recoils. Volume of breath 0.5 Volume of breath. During each breath, the pressure gradients move 0.5 liter of air into and out of the lungs. 0 Volume (L) 5 seconds elapsed © 2016 Pearson Education, Inc. 21 Physical Factors Influencing Respiration Three physical factors influence the ease of air passage and the amount of energy required for ventilation – Airway resistance: size of the airways offers some resistance to air flow, most resistance in mid size bronchi – Alveolar surface tension: fluid in alveoli creates surface tension that tend to inhibit alveoli expansion. Surfactant a mix of detergent like lipid and protein from type 2 alveolar cells reduce this surface tension – Lung and thoracic wall compliance: if tissue have reduced compliance (elasticity) it will increase the effort necessary to expand the thorax and the lungs, could be caused by: Non elastic scar tissue replacing lung tissue (fibrosis) Reduced production of surfactant Decreased flexibility of thoracic cage 22 11.
Scene 12 (14m 18s)
[Audio] 2025-03-04 Respiratory imbalances As airway resistance rises, breathing movements become more strenuous, severe constriction or obstruction of bronchioles: Can prevent life sustaining ventilation Can occur during acute asthma attacks and stop ventilation – Epinephrine/salbutamol dilates bronchioles, reduces air resistance Insufficient quantity of surfactant in premature infants causes infant respiratory distress syndrome and results in collapse of alveoli after each breath – Treatment: spraying natural or synthetic surfactant into newborn’s air passages, and use of positive pressure devices also help to keep alveoli open between breaths Compliance of the thoracic wall can be affected by deformities of thorax, ossification of costal cartilage, and paralysis of intercostal muscles 23 Assessing Ventilation Respiratory volumes can be used to assess respiratory status Respiratory volumes can be combined to calculate respiratory capacities, to inform on a person’s respiratory status and pulmonary disorders A spirometer can measure patient’s respiratory volumes 24 12.
Scene 13 (15m 30s)
[Audio] 2025-03-04 Respiratory Volumes and Capacities Tidal volume (T-V---): amount of air moved into and out of lung with each breath ~500ml Inspiratory reserve volume (I-R-V--): amount of air that can be inspired forcibly beyond the tidal volume (2100–3200 ml) Expiratory reserve volume (E-R-V--): amount of air that can be forcibly expelled from lungs (1000–1200 ml) Residual volume (R-V---): amount of air that always remains in lungs to keep alveoli open Capacities are combinations of two or more respiratory volumes – Inspiratory capacity (I-C---): TV plus I-R-V – Functional residual capacity (F-R-C--): RV plus E-R-V – Vital capacity (V-C---): TV plus I-R-V plus E-R-V – Total lung capacity (T-L-C--): sum of all lung volumes (TV plus I-R-V plus E-R-V plus RV) 25 Dead Space Anatomical dead space: does not contribute to gas exchange – Consists of air that remains in passageways ~150 ml out of 500 ml TV Alveolar dead space: space occupied by nonfunctional alveoli due to collapse or obstruction Total dead space: sum of anatomical and alveolar dead space 26 13.
Scene 14 (16m 59s)
[Audio] 2025-03-04 Gas Exchange Gas exchange occurs between lungs and blood as well as blood and tissues External respiration: diffusion of gases between blood and lungs Internal respiration: diffusion of gases between blood and tissues Both processes are subject to: – Basic properties of gases – Composition of alveolar gas 27 Basic Properties of Gases Dalton’s law of partial pressures – Total pressure exerted by mixture of gases is equal to sum of pressures exerted by each gas – Partial pressure is pressure exerted by each gas in mixture and is directly proportional to its percentage Total atmospheric pressure equals 760 millimeters Hg Nitrogen makes up ~78.6% of air; partial pressure of nitrogen, P-N-2--, can be calculated: 0.786 760 millimeters Hg 597 millimeters Hg O2 is 20.9% of air, P-O-2 equals: 0.209 760 millimeters Hg 159 millimeters Hg 28 14.
Scene 15 (18m 11s)
[Audio] 2025-03-04 Basic Properties of Gases Air also contains 0.04% C-O-2--, 0.5% water vapor, and insignificant amounts of other gases At high altitudes, partial pressures declines, but at lower altitudes (under water), partial pressures increase significantly Sea level High Altitude 29 Henry’s law – Gas mixtures in contact with liquids: each gas will dissolve in the liquid in proportion to its partial pressure – At equilibrium, partial pressures in both phases will be equal – Amount of each gas that will dissolve depends on: – Solubility: C-O-2 is 20 more soluble in water than O2, and little N2 will dissolve – Temperature: increases in liquid temperature cause solubility to decreases 30 15.
Scene 16 (19m 4s)
[Audio] 2025-03-04 Composition of Alveolar Gas Alveoli contain more C-O-2 and water vapor than atmospheric air because of: – Gas exchanges in lungs (O2 diffuses from alveoli to blood, C-O-2 diffuses in opposite direction) – Humidification of air by conducting passages – Mixing of alveolar gas with each breath as newly inspired air mixes with air that was left in passageways between breaths 31 Partial pressure gradients and gas movements in the body. 32 16.
Scene 17 (19m 35s)
[Audio] 2025-03-04 External Respiration External respiration (pulmonary gas exchange) involves exchange of O2 and C-O-2 across respiratory membranes Exchange is influenced by: – Partial pressure gradients and gas solubilities – Thickness and surface area of respiratory membrane – Ventilation perfusion coupling: matching of alveolar ventilation with pulmonary blood perfusion 33 Partial pressure gradients and gas solubilities Steep partial pressure gradient for O2 between blood and lungs: Venous blood PO2 = 40 millimeters Hg against Alveolar PO2 = 104 millimeters Hg – Drives oxygen flow into blood, equilibrium is reached in ~0.25 seconds, but it takes RBC ~0.75 seconds to travel from start to end of pulmonary capillary. Ensures adequate oxygenation even if blood flow increases 3 Partial pressure gradient for C-O-2 is less steep: – Venous blood PCO2 =45 millimetersHg against Alveolar PCO2 =40 millimetersHg – Though gradient is smaller, C-O-2 still diffuses in equal amounts with oxygen because C-O-2 is 20 more soluble than oxygen 34 17.
Scene 18 (20m 55s)
[Audio] 2025-03-04 Respiratory membrane thickness & surface area Respiratory membranes are very thin ~0.5 to 1 m Large total surface area of alveoli: 40 the surface area of the skin Effective thickness of respiratory membrane increases dramatically if lungs fluid filled such as seen in pneumonia or left heart failure – The time R-B-C's spend in transit through pulmonary capillaries may not be enough for adequate gas exchange – Can cause body tissues to suffer from oxygen deprivation Certain pulmonary diseases drastically reduce alveolar surface area – In emphysema, walls of adjacent alveoli break down, and alveolar chambers enlarge Tumors, mucus, or inflammatory material also can reduce surface area by blocking gas flow into alveoli 35 Ventilation perfusion coupling – Perfusion: blood flow reaching alveoli – Ventilation: amount of gas reaching alveoli – Ventilation and perfusion rates must be matched for optimal, efficient gas exchange – Controlled by local autoregulatory mechanisms PO2 controls perfusion by changing arteriolar diameter PCO2 controls ventilation by changing bronchiolar diameter – Balancing ventilation and perfusion Changing diameters of local arterioles and bronchioles synchronizes ventilation perfusion Ventilation perfusion is never balanced for all alveoli because: 1. Regional variations may be present, due to effect of gravity on blood and air flow 2. Occasionally, alveolar ducts plugged with mucus cause unventilated areas 36 18.
Scene 19 (22m 38s)
[Audio] 2025-03-04 O2 and C-O-2 influence on ventilation/perfusion – Influence of local P-O-2 on perfusion Changes in P-O-2 in alveoli cause changes in arteriolar diameters Where alveolar O2 is high, arterioles dilate – Where alveolar O2 is low, arterioles constrict – Directs blood to go to alveoli, where oxygen is high, to pick up more oxygen Opposite mechanism seen in systemic arterioles that dilate when oxygen is low and constrict when high – Influence of local P-C-O-2 on ventilation Changes in P-C-O-2 in alveoli cause changes in diameters of bronchioles – Where alveolar C-O-2 is high, bronchioles dilate – Where alveolar C-O-2 is low, bronchioles constrict – Allows elimination of C-O-2 more rapidly 37 Internal Respiration Internal respiration is capillary gas exchange in body tissues Partial pressures and diffusion gradients are reversed compared to external respiration – Tissue P-O-2 is always lower than in arterial blood P-O-2 (40 against 100 millimeters Hg), so oxygen moves from blood to tissues – Tissue P-C-O-2 is always higher than arterial blood P-C-O-2 (45 against 40 millimeters Hg), so C-O-2 moves from tissues into blood – Venous blood returning to right ventricle has P-O-2 of 40 millimeters Hg and P-C-O-2 of 45 millimeters Hg 38 19.
Scene 20 (24m 20s)
[Audio] 2025-03-04 Oxygen Transport in Blood O2 is carried in blood in two ways: – 1.5% is dissolved in plasma – 98.5% is reversibly bound to each Fe of hemoglobin (Hb) in RBCs Association of oxygen and hemoglobin – Each Hb molecule is composed of four polypeptide chains, each with an iron containing heme group, each Hb can transport up to four oxygen molecules – Oxyhemoglobin (HbO2): hemoglobin O2 combination – Reduced hemoglobin (deoxyhemoglobin) (HHb): hemoglobin that has released O2 39 Association of oxygen and hemoglobin Loading and unloading of O2 facilitated by Hb change in shape – As O2 binds, Hb changes shape, increasing its affinity for O2 – As O2 released, Hb shape change and has lower affinity for O2 – Fully saturated (100%): all four heme groups carry O2 – Partially saturated: when only one to three hemes carry O2 Rate of loading and unloading of O2 is regulated for adequate delivery to cells 40 20.
Scene 21 (25m 34s)
[Audio] 2025-03-04 Association of oxygen and hemoglobin Loading and unloading of O2 facilitated by Hb change in shape – As O2 binds, Hb changes shape, increasing its affinity for O2 – As O2 released, Hb shape change and has lower affinity for O2 – Fully saturated (100%): all four heme groups carry O2 – Partially saturated: when only one to three hemes carry O2 Rate of loading and unloading of O2 is regulated for adequate delivery to cells Several physiological factors influence hemoglobin saturation Regulation of hemoglobin saturation is optimized to maintain homeostasis: Promote O2 loading at lungs Promote O2 unloading at tissues 41 Influence of P-O-2 on hemoglobin saturation PO2 strongly influences binding/release of O2 with hemoglobin % of Hb saturation can be plotted against P-O-2 concentrations: oxygen hemoglobin dissociation curve. relationship is not linear, but sigmoid (S-shaped) curve 42 21.
Scene 22 (26m 43s)
[Audio] 2025-03-04 Influence of P-O-2 on hemoglobin saturation In arterial blood P-O-2 is 100 millimeters Hg and contains 20 ml of oxygen per 100 ml blood: Hb is 98% saturated – Further increases in P-O-2 (as in deep breathing) produce minimal increases in O2 binding In venous blood, P-O-2 is 40 millimeters Hg and Hb is still 75% saturated – Venous reserve: oxygen remaining in venous blood that can still be used 43 © 2016 Pearson Education, Inc. 44 22.
Scene 23 (27m 27s)
[Audio] 2025-03-04 © 2016 Pearson Education, Inc. 45 Influence of other factors on Hb saturation Increases in temperature, H plus , P-C-O-2-, and B-P-G (biphosphoglycerate) alter structure of hemoglobin, decreasing Hb’s affinity for O2 – Occurs in systemic capillaries and enhances O2 unloading, causing a shift in O2-hemoglobin dissociation curve to right Decreases in these factors shift curve to left and decreases oxygen unloading from blood Bohr effect: CO2/pH effect on O2 loading 46 23.
Scene 24 (28m 10s)
[Audio] 2025-03-04 Bohr effect, Biphosphoglycerate As cells metabolize glucose, they use O2, causing: – Increases in P-C-O-2 and H plus , lactic acid in capillary blood – Declining blood pH (acidosis) and increasing Pco2 cause HbO2 bond to weaken: the Bohr effect » O2 unloading occurs where needed most – Heat production in active tissue directly and indirectly (R-B-C--) decreases Hb affinity for O2 » Allows increased O2 unloading to active tissue Androgens, epinephrine, thyroid hormones, and growth hormone activate R-B-C's and make them produce biphosphoglycerate (B-P-G--) as a by product of glycolysis, also cause decrease in Hb affinity 47 Hypoxia Hypoxia: inadequate O2 delivery to tissues; can result in cyanosis Hypoxia is based on cause: – Anemic hypoxia: too few R-B-C-s-, abnormal, too little Hb – Ischemic hypoxia: impaired or blocked circulation – Histotoxic hypoxia: cells unable to use O2, as in metabolic poisons – Hypoxemic hypoxia: abnormal ventilation; pulmonary disease – Carbon monoxide poisoning: especially from fire Hb has a 200 greater affinity for carbon monoxide than oxygen 48 24.
Scene 25 (29m 45s)
[Audio] 2025-03-04 Carbon Dioxide Transport C-O-2 is transported in blood in three forms: – 7 to 10% is dissolved in plasma as P-C-O-2 – 20% of C-O-2 is bound to the globin part of hemoglobin: carbaminohemoglobin –) in plasma – 70% is transported as bicarbonate ions (HCO3 Formation of bicarbonate involves C-O-2 combining with water to form carbonic acid (H2CO3), which quickly dissociates into bicarbonate and H plus 49 Transport and exchange of C-O-2 and O2. Tissue cell Interstitial fluid C-O-2 C-O-2 (dissolved in plasma) Binds to plasma proteins H Slow C-O-2 Co2 H2o H2co3 H-C-O-3 C-O-2 H-C-O-3 Cl Fast Cl H-C-O-3 C-O-2 H H2CO3 CO2 H-2-O Chloride shift (in) via transport protein Carbonic anhydrase C-O-2 Hhb Co2 CO2 Hb HbCO2 (Carbaminohemoglobin) HbO2 O2 Hb Red blood cell C-O-2 O2 O2 (dissolved in plasma) Blood plasma O2 Oxygen release and carbon dioxide pickup at the tissues © 2016 Pearson Education, Inc. 50 25.
Scene 26 (31m 47s)
[Audio] 2025-03-04 Transport and exchange of C-O-2 and O2. Alveolus Fused basement membranes C-O-2 C-O-2 (dissolved in plasma) Slow H C-O-2 H-C-O-3 Co2 H2o H2co3 H-C-O-3 Cl Fast C-O-2 H-C-O-3 H H2CO3 CO2 H-2-O Chloride shift (out) via transport protein Carbonic anhydrase Cl C-O-2 CO2 Hb HbCO2 (Carbaminohemoglobin) HbO2 H O2 HHb Red blood cell O2 O2 Blood plasma O2 (dissolved in plasma) Oxygen pickup and carbon dioxide release in the lungs © 2016 Pearson Education, Inc. 51 Carbon Dioxide Transport Occurs primarily in R-B-C-s-, where enzyme carbonic anhydrase reversibly and rapidly catalyzes this reaction – is created, it quickly In systemic capillaries, after H-C-O-3 – from R-B-C's is balanced as Cl– moves into diffuses from R-B-C's into plasma – Outrush of H-C-O-3 R-B-C's from plasma: chloride shift In pulmonary capillaries, the processes is reversed – imported into R-B-C's and Cl excreted back into plasma – H-C-O-3 – H-C-O-3 – binds with H plus to form H2CO3 – H-2-C-O-3 is split by carbonic anhydrase into C-O-2 and water – C-O-2 diffuses into alveoli 52 26.
Scene 27 (33m 20s)
[Audio] 2025-03-04 Haldane effect – Amount of C-O-2 transported is affected by P-O-2 – The lower the P-O-2 and hemoglobin O2 saturation, the more C-O-2 can be carried in blood – Reduced hemoglobin buffers H plus , forms carbaminohemoglobin more easily – Process encourages C-O-2 exchange at tissues and at lungs At tissues, as more C-O-2 enters blood, more oxygen dissociates from hemoglobin (Bohr effect) As HbO2 releases O2, it more readily forms bonds with C-O-2 to form carbaminohemoglobin (Haldane effect) 53 Influence of C-O-2 on blood pH – Carbonic acid–bicarbonate buffer system: helps blood resist changes in pH If H plus concentration in blood rises, excess H plus combines with H-C-O-3 – to form H2CO3, which dissociates into C-O-2 and H2O If H plus concentration drops, H-2-C-O-3 dissociates, releasing H plus – is the alkaline reserve of carbonic acid bicarbonate HCO3 buffer system Changes in respiratory rate and depth affect blood pH – Slow, shallow breathing causes an increase in C-O-2 in blood, resulting in a drop in pH: acidosis – Rapid, deep breathing causes a decrease in C-O-2 in blood, resulting in a rise in pH Changes in ventilation can help adjust pH when disturbances are caused by metabolic factors – Breathing plays a major role in acid base balance of body 54 27.
Scene 28 (35m 0s)
[Audio] 2025-03-04 Control of Respiration Respiratory rhythms are regulated by higher brain centers, chemoreceptors, and other reflexes Neural controls involve neurons in reticular formation of medulla and pons Medullary respiratory centers: 1. Ventral respiratory group (V-R-G--): Rhythm generating integrative center in brain stem from spinal cord to pons medulla junction Sets eupnea: normal respiratory rate and rhythm (12–15 breaths/min) Its inspiratory neurons excite inspiratory muscles via phrenic (diaphragm) and intercostal nerves (external intercostals) Expiratory neurons inhibit inspiratory neurons 2. Dorsal respiratory group (D-R-G--) Network of neurons located near root of cranial nerve 9 Group integrates input from peripheral stretch and chemoreceptors, then sends information to V-R-G neurons 55 Pontine respiratory centers – Neurons in this center influence and modify activity of V-R-G – Act to smooth out transition between inspiration and expiration and vice versa – Transmit impulses to V-R-G that modify and fine tune breathing rhythms during vocalization, sleep, exercise – Lesions in this area of brain lead to apneustic breathing, where patient takes prolonged inspirations 56 28.
Scene 29 (36m 28s)
[Audio] 2025-03-04 Factors Influencing Breathing Rate and Depth Depth is determined by how actively respiratory center stimulates respiratory muscles – The greater the stimulation, the greater the number of motor units excited, increasing depth of inspiration Rate is determined by how long center is active Both are modified by changing body demands Respiratory centers are affected by: – Chemical factors – Influence of higher brain centers – Pulmonary irritant reflexes – Inflation reflex 57 Chemical factors – Most important of all factors affecting depth and rate of inspiration – Changing levels of P-C-O-2-, P-O-2--, and pH are most important – Levels of these chemicals are sensed by: Central chemoreceptors: located throughout brain stem Peripheral chemoreceptors: in aortic arch and carotid arteries PCO2 is most potent and most closely controlled, if blood P-C-O-2 levels rise (hypercapnia), C-O-2 accumulates in brain and joins with water to become carbonic acid – Carbonic acid dissociates, releasing H plus , causing a drop in pH – Increased H plus stimulates central chemoreceptors of brain stem, which synapse with respiratory regulatory centers – Respiratory centers increase depth and rate of breathing, which act to lower blood P-C-O-2-, and pH rises to normal levels If blood P-C-O-2 levels decrease, respiration becomes slow, shallow Apnea: breathing cessation when P-C-O-2 levels drop abnormally low 58 29.
Scene 30 (38m 13s)
[Audio] 2025-03-04 Changes in P-C-O-2 regulate ventilation by a negative feedback mechanism. Arterial P-C-O-2 PCO2 decreases pH in brain extracellular fluid (E-C-F--) Peripheral chemoreceptors in carotid and aortic bodies (mediate 30% of the C-O-2 response) Central chemoreceptors in brain stem respond to H in brain E-C-F (mediate 70% of the C-O-2 response) Afferent impulses Medullary respiratory centers Efferent impulses Respiratory muscle Ventilation (more C-O-2 exhaled) Initial stimulus Physiological response Arterial P-C-O-2 and pH return to normal Result © 2016 Pearson Education, Inc. 59 Hyperventilation Increased depth and rate of breathing that exceeds body’s need to remove C-O-2 – May be caused by anxiety attacks – Leads to decreased blood C-O-2 levels (hypocapnia) Causes cerebral vasoconstriction and cerebral ischemia, resulting in dizziness, fainting Early symptoms include tingling and involuntary muscle spasms in hands and face – Treatment: breathing into paper bag increases C-O-2 levels being inspired 60 30.
Scene 31 (39m 36s)
[Audio] 2025-03-04 Influence of P-O-2 Peripheral chemoreceptors in aortic and carotid bodies sense arterial O2 levels Declining P-O-2 normally has only slight effect on ventilation because of huge O2 reservoir bound to Hb – Requires substantial drop in arterial P-O-2 (below 60 millimeters Hg) to stimulate increased ventilation – When excited, chemoreceptors cause respiratory centers to increase ventilation 61 Influence of arterial pH pH can modify respiratory rate and rhythm even if C-O-2 and O2 levels are normal Mediated by peripheral chemoreceptors Decreased pH may reflect C-O-2 retention, accumulation of lactic acid, or excess ketone bodies Respiratory system controls attempt to raise pH by increasing respiratory rate and depth (see Acid Base regulation chapter) 62 31.
Scene 32 (40m 42s)
[Audio] 2025-03-04 Summary of chemical factors Rising C-O-2 levels are most powerful respiratory stimulant Normally, blood P-O-2 affects breathing only indirectly by influencing peripheral chemoreceptor sensitivity to changes in P-C-O-2 When arterial P-O-2 falls below 60 millimeters Hg, it becomes major stimulus for respiration (via peripheral chemoreceptors) Changes in arterial pH resulting from C-O-2 retention or metabolic factors act indirectly through peripheral chemoreceptors 63 Brain centers and reflexes – Hypothalamic controls: act through limbic system to modify rate and depth of respiration Ex: breath holding that occurs in anger or gasping with pain Change in body temperature changes rate – Cortical controls bypass medullary controls and direct signals from cerebral motor cortex. Ex: voluntary breath holding at least until brain stem reinstates breathing when blood C-O-2 becomes critical – Pulmonary irritant reflexes: receptors in bronchioles respond to irritants (dust, mucus, toxic fumes) – Receptors signal respiratory centers via vagal nerve afferents Promote reflexive constriction of air passages Same irritant triggers a cough in trachea or bronchi or a sneeze – Inflation reflex: Hering Breuer reflex (inflation reflex): stretch receptors in pleurae and airways are stimulated by lung inflation and send inhibitory signals to medullary respiratory centers to end inhalation and allow expiration. Not important under normal condition 64 32.
Scene 33 (42m 31s)
[Audio] 2025-03-04 Neural and chemical influences on brain stem respiratory centers. 65 Exercise respiratory Adjustments During exercise, adjustments geared to both intensity and duration must be made Hyperpnea: increased ventilation in response to metabolic needs: ventilation can increase 10 to 20 fold Ventilation increases abruptly, then gradually, and then reaches steady state; when exercise stops, there is a small, abrupt decline in ventilation, followed by a gradual decrease PCO2, P-O-2--, and pH remain surprisingly constant during exercise Abrupt increase in ventilation that occurs as exercise begins involves three neural factors: 1. Psychological stimuli: anticipation of exercise 2. Simultaneous cortical motor activation of skeletal muscles and respiratory centers 3. Excitatory impulses to respiratory centers from proprioceptors in moving muscles, tendons, joints – Gradual increase and plateau of respiration is caused by increased rate of C-O-2 delivery to the lungs 66 33.
Scene 34 (43m 45s)
[Audio] 2025-03-04 Exercise respiratory Adjustments Ventilation declines suddenly as exercise ends is because the three neural factors are shut off – Gradual decline to baseline is due to decline in C-O-2 flow after exercise ends Exercise leads to anaerobic respiration and formation of lactic acid – Lack of oxygen in muscles is not from poor respiratory function, but rather from insufficient cardiac output or skeletal muscle inability to increase oxygen uptake 67 34.